
Virtual Reality: Healthcare and Biomedical Research
Overview Virtual reality was first experienced as the world’s first flight stimulator Link Trainer by Edwin Link (1929) and later as the interactive theatre ‘Sensorama’

Asthma is a chronic respiratory disease affecting millions of people worldwide and has a global economic burden of more than 50 billion dollars. Asthma patients suffer from shortness of breath, chest tightness, coughing and wheezing, all of which needs to be managed life-long. Although asthma cannot be treated, it can be kept under control by a combination of drugs including Beta-blockers, corticosteroids, leukotriene modifiers etc.
Asthma is a globally prevalent condition that has been a hot topic for research for decades. Traditionally, data collection on asthma has been a complicated process requiring investigations from multiple resources. Some of the sources for data collection include:
These processes require long duration, diligence and large manpower. Such data may still be inaccurate or lost due to the long complicated process. However, in the era of digitization, data collection can be done by much simpler and more convenient methods.
Installation of free applications on the mobile phone of patients can be done to collect data [1] on asthma prevalence, activity limitation, days of work or school lost, rescue and control medication use, asthma self-management education, physician visits, emergency department visits and hospitalizations due to asthma. Data collected using digital tools are not only convenient but also significantly improve accuracy.
Incorporating the use of sensors and data recording while examining patients in the outpatient department during regular general physicians visit can be another useful data collection method for an asthma study. Along with this, adding sensors with automatic data collection digital tools to home-based self-management applications could also be used for asthma study purposes.
The available digital tools can have two major applications. It can be used to collect data for asthma research and can also be used as a guide for physicians on any required changes in treatment modalities. These tools can assess information on episodes of acute exacerbations, the number of hospital visits, patient knowledge of inhaler techniques, and overall epidemiology of asthma prevalence. These tools are not only beneficial for the patients, but they also are excellent for researching patient demographics and patients’ medical compliance at home. They can also help physicians better educate their patients by understanding the mistakes asthma patients make when it comes to using their medications at home without a doctor’s assistance. The main purpose of this article is to educate researchers on the various digital health tools that are used to study asthma and how it can be useful to them.
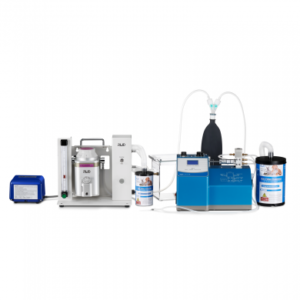
A new innovative technology, electronic inhalers equipped with sensors has been recently gaining popularity for its ability to accurately record data. This technology also has great potential as a tool in studying asthma for research.
Electronic sensors combined with inhalers can be highly useful to document a patient’s progress before and after treatment. This can be done by monitoring the spirometry values, detecting the frequency of inhaler use, and the time period of peak use.
Electronic inhaler sensors were used in a study[4] to track medication usage as well as gather information by acting as an effective digital tool to conduct studies on asthma treatment and efficacy. The study analyzed asthma control, device usability, user-friendly nature and value of the technology. It concluded that electronic sensors combined with a digital health platform had reports of high customer satisfaction. Most patients perceive high value in such devices and sought long-term continued use of digital health platforms for asthma control. Ease of use and convenience was found to be a major influencing factor amongst patients’ preference for continued usage of the digital tools.
Similarly, in another study,[5] residents of a specific area with asthma received electronic inhaler sensors which assessed medication dosage, time and frequency of medication required for a period of 30 days. After completion of the 30-day mark, patients took part in a self-management digital health intervention to enhance at home treatment and prevention of asthma episodes. The study analyzed the progress achieved in outcomes by taking into account the number of daily Short Acting Beta Agonists (SABA), days with and without symptoms, and the degree of control over asthma through a period starting from the initial 30-day baseline to the following months. A significant improvement was observed with a 39% reduction in the mean number of SABA event, and 12% increment in the number of days without symptoms. This improvement was observed to increase over time in the subsequent months with an overall improvement in asthma control.
Recently, Sema4, a patient-centered predictive health company, and the Mount Sinai Health System have collaborated with Sanofi on a five-year study of almost 1,200 asthma patients. The study was developed to analyze the potential in incorporating digital tools to collect research data on Asthma. It will employ connected apps with sensors to analyze the difference in the effects of asthma on different individuals while also collecting clinical, genomic and environmental data.
Currently, there are many apps with varying functions to assess data from patients regarding asthma symptoms, exacerbations and their management. Vigorous study and evaluation are required to assess the feasibility of using mobile applications as a tool to obtain data for clinical studies.
A wide scale study was initiated in 2015 using an application that was uploaded on the apple store. Since the beginning of the research, this application has been downloaded by more than 50,000 iPhone users. The app collected information via surveys on the varying ways asthma patients dealt with their disease, as well as the various treatments methods employed by each patient. The results of the study were compared to a control group of asthma patients to analyze the accuracy of patient-reported data. Further details into the research such as research objectives, data collected, potential, methodology, have been described below.[2]
Target Population
Individuals over 18 with asthma confirmed by a doctor, taking medications for asthma, not pregnant and living in the United States.
Total Participants
7,593
Methodology
The study collected data remotely via smartphones from 7,593 participants that included many patients with severe asthma via
Research Objectives
Data collected
The data collection was multidimensional using mediums such as surveys and devices over a period of 6 months. Data were collected on patients regarding their asthma triggers, geolocation, and air quality of their location. These data were collected by obtaining information inputted manually by the patients, acquiring patient’s geolocation information via their mobile GPS, and through surveys.
Study Findings
Initial study results reported heat, pollen and wildfires to be significant triggers for asthma exacerbation episodes. The study’s multidimensional data collection method enabled high quality collection of data by correlating interrelated variables.
Dr. Sam Pejham is a pediatric specialist who developed a free application- AsthmaMD that allows users to manually log their asthma activity, their medications and triggers of their asthma in the form of a diary. The app was designed with the intention of researching the risk factors that trigger asthma and the potential ways to avoid them. In addition to this, the study assesses the effectiveness of different medication dosage during each asthma episode and the frequency of asthma exacerbation. Let us look further into the study with a short description of each aspect of the research.[3]
Target Population
Asthma patients of all ages across the world
Methodology
The application keeps a record of asthma patients by allowing patients to manually record their asthma activity, their medications and causes of their asthma as a medical journal.
Data collected
Potential
AsthmaMD is designed to help asthma patients while also gathering anonymous data to aid researchers with information about the causes and external correlation of asthma. It also solves the issue of privacy by allowing AsthmaMD users to optionally opt-in and to allow the application to securely send encrypted and anonymous data.
The PRAM was designed by the Ontario Lung Association with dual purposes. The app assists patients in self-managing their asthma and collects data for research purposes. It uses a scoring system to analyze the severity of symptoms and provide a plan for acute care. Here are the available details regarding the app’s potential for research purposes.
Target Population
Pediatric Asthma patients (1-17 years old)
Methodology
It rapidly calculates a score based on clinical findings recorded by the patient into the platform. The collected data then provides the score which gives an idea about the level of asthma severity.
Data collected
PRAM employs a scoring system of 12 points to objectively assess the degree of asthma severity. It collects information on 5 major clinical findings in episodes of acute exacerbation including oxygen saturation, suprasternal retractions, scalene muscle use, air entry and wheezing.
Potential
Offered by Ontario lung association,Since 2015, within the first 3 years of release, this app had over 1000 downloads and is still available for download. It can aid researchers to obtain information on patient’s condition and treatment methodology during acute exacerbation. Although no study has yet been conducted regarding the effectiveness of the app, it shows potential in being utilized as a tool for collecting data for research purposes.
SaniQ asthma allows patients to record their medical data in the form of a daily medical journal. Individualized data collection allows the collection of data in a more accurate manner by removing subjective data collector bias. Although no study has yet been conducted on the usage of this app for research, it shows some promising potential as a digital tool for study. The following information can further aid in understanding the app’s effectiveness as a research tool.
Target Population
Asthma patients of all ages across the world
Methodology
SaniQ asthma app allows patients to record their medical data in the form of a daily medical journal.
Data collected
Potential
The individualized data collection allows the collection of data in a more accurate manner by removing subjective data collector bias. Data collected by such methods greatly reduce research costs, labor and time.
The major limitations in using digital tools to study asthma include
Digital tools enhance the widespread involvement of participants by eliminating limitations of geographical barriers, facilitating multi-dimensional assessments, and collecting objective data. As smartphone usage and technological advancement is increasing globally, the use of digital tools in Asthma study has huge potential.

Overview Virtual reality was first experienced as the world’s first flight stimulator Link Trainer by Edwin Link (1929) and later as the interactive theatre ‘Sensorama’

Episodic Memory Human long-term memory can be broadly classified into declarative memory and procedural (implicit) memory; The former category involves conscious and intentional recollection of
Self-Awareness Consciousness by most of the scientific community is recognized as an outward awareness of one’s environment and body, while self-awareness is the recognition of

Need Digital Health Services for your research? Click here Questionnaires, Data Forms & Research Medical research and data go hand in hand. Often, to





DISCLAIMER: ConductScience and affiliate products are NOT designed for human consumption, testing, or clinical utilization. They are designed for pre-clinical utilization only. Customers purchasing apparatus for the purposes of scientific research or veterinary care affirm adherence to applicable regulatory bodies for the country in which their research or care is conducted.