

With the increasing role of patient-reported outcome measures in today’s digital health industry, rating scales are among the most effective tools used to assess subjective experiences, such as pain, mood, appetite, and comfort with knowledge. Rating scales facilitate the collection of qualitative and quantitative data in research, which can be used to track the progression of a condition or response to treatment. In fact, subjective scales improve the diagnostic process in practice, as well as data interoperability.
Thus, rating scales become fundamental to data collection and patients’ health-related quality of life. Some of the most popular and reliable rating scales include the visual analog scale, the verbal rating scale, the faces rating scale, and the numeric rating scale. Moreover, the use of electronic rating scales (delivered via a web-based platform, mobile devices or interactive voice record technology) results in high compliance and a positive user experience.
Rating scales are valuable tools in digital health and routine clinical care, used to assess a variety of subjective phenomena, such as fatigue, user satisfaction, asthma, and even provider performance. Interestingly, such measurements are most often applicable to pain assessment and pain management. Common rating scales with high psychometric properties and a wide range of applications include the visual analog scale, the verbal rating scale, the faces rating scale, and the numeric rating scale, as well as their electronic versions:
Rating scales, such as the verbal rating scale, the numeric rating scale, and the visual analog scale, reveal good psychometric properties and meet fundamental regulatory requirements for pain assessment. As rating scales cannot be replaced or used interchangeably, choosing the right measurement can be challenging. The selection of a tool depends on study conditions, such as demographic factors, methods of administration, instructions, specific circumstances, and interpretation of clinical significance (Williamson and Hoggart, 2005). That said, although clear comparisons between rating scales cannot be made, evidence suggests:
While research proves that all rating scales work well, the interpretation of patients’ scores is crucial. For instance, using raw scores to assess pain reduction may lead to error. To set an example, a change from 51 to 48 mm on a 100-mm visual analog scale is a change of 6%. On a 0-10 numeric scale, this can be represented as a change from 5 to 4, which, however, is a change of 20%. Therefore, multidimensional assessments are also needed to evaluate a patient’s subjective experience with all its psychological, social, and financial aspects.
With their numerous applications in practice, rating scales are among the most popular subjective measures employed in pain assessment. Note that a comprehensive pain assessment tackles the unidimensional evaluation of pain intensity and the multidimensional assessment of a patient’s pain perception. Rating scales, in particular, provide a quick and reliable way to assess the unidimensional pain intensity regarding the area of pain or specific circumstances (e.g., hip pain when sitting). As pain is a complex and internal phenomenon, the vast majority of pain experiences cannot be detected by standard observations or laboratory tests. Thus, only self-reports can help experts understand, evaluate, and treat both acute and chronic pain.
Given the multidimensional aspect of pain, each rating scale has various benefits in pain assessment, which is the main key to effective treatment. Acute pain, for instance, can be caused by an injury or disease and serves a biological purpose. In order to be reduced in an effective manner, evidence shows that acute pain should be documented within the first 20-25 minutes of the initial assessment in the emergency department. Note that treatment should tackle the underlying cause of a patient’s sensory experience (Karcioglu et al., 2018). Chronic pain, on the other hand, is defined as pain lasting more than 12 weeks with no recognizable end point. As chronic pain is perceived as a disease itself, treatment must embrace a multidisciplinary approach and multidimensional measures. Rating scales facilitate both the evaluation of pain and its comprehensive assessment.
Rating scales are popular instruments in pain assessment, with verbal rating scales, visual analog scales, and numeric rating scales being valid and reliable tools in health care. Subjective measures can help experts evaluate factors, such as location and nature of pain. Note that pain is a complex experience and may be influenced by demographic factors and social pressure. In fact, beliefs, cultural differences, and expectations have an impact on patients’ experiences. Fear and anxiety, for instance, may lead to an increase in pain intensity. When assessing pain, there are several major factors to consider:
Rating scales are popular subjective instruments used to assess abstract events and internal experiences, such as food intake, emotional arousal to daily activities, asthma, and service satisfaction. While there’s a potential for error within ratings, rating scales (such as the verbal rating scale, the numeric rating scale, the visual analog scale, and the faces rating scale) are valid and reliable tools in medical research and routine clinical care. Such measurements reveal numerous benefits and applications across a wide variety of settings and populations; particularly in pain assessment. As pain, described as the fifth vital sign, is one of the biggest health concerns worldwide, rating scales are commonly employed alongside other multifaceted patient-reported measurements.
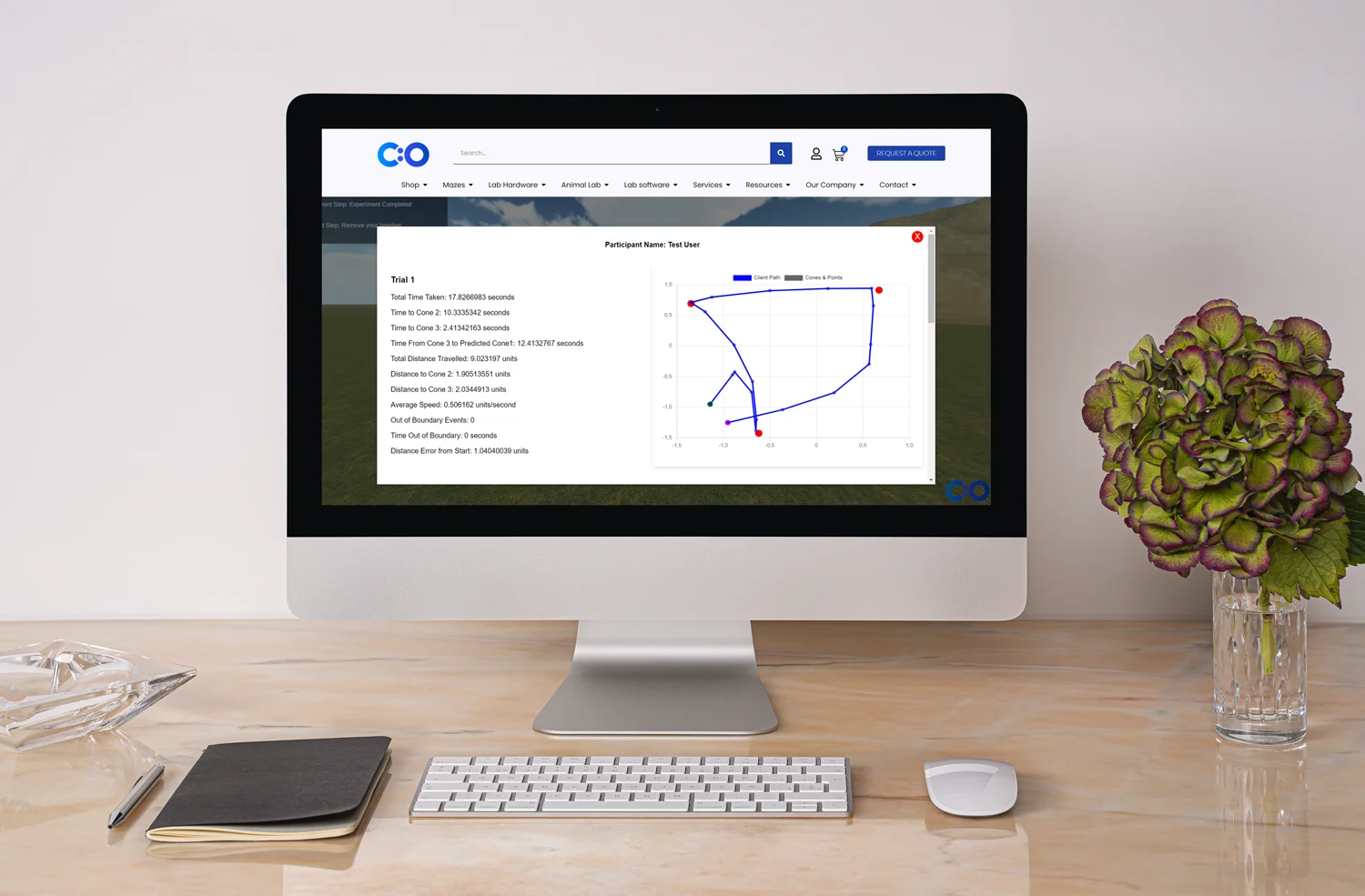
What’s more, with the leveraging role of health technologies in today’s health care industry, electronic rating scales are becoming more and more popular. Digital tools improve data collection and analysis, as well as interoperability. After all, patients are active participants in today’s digital health world – with the right to voice their subjective experience and opt for high health-related quality of life.








Dr Louise Corscadden acts as Conduct Science’s Director of Science and Development and Academic Technology Transfer. Her background is in genetics, microbiology, neuroscience, and climate chemistry.
