Parkinson’s disease (PD) is the most common neurological disorder that is characterized by debilitating motor abnormalities, including muscle rigidity, resting tumor, stiffer voluntary movements, and postural instability. Primary neuropathological condition of PD includes progressive degeneration of the dopaminergic neurons in the nigrostriatal area. Experimental models of PD are specifically designed to gain detailed insights into the pathological mechanisms of the disease. In addition to this function, animal models are essential in the development and evaluation of new therapeutic molecules and strategies. The introduction of the catecholamine neurotoxin 6-hydroxydopamine (6-OHDA) has revolutionized the research in Parkinsonism.
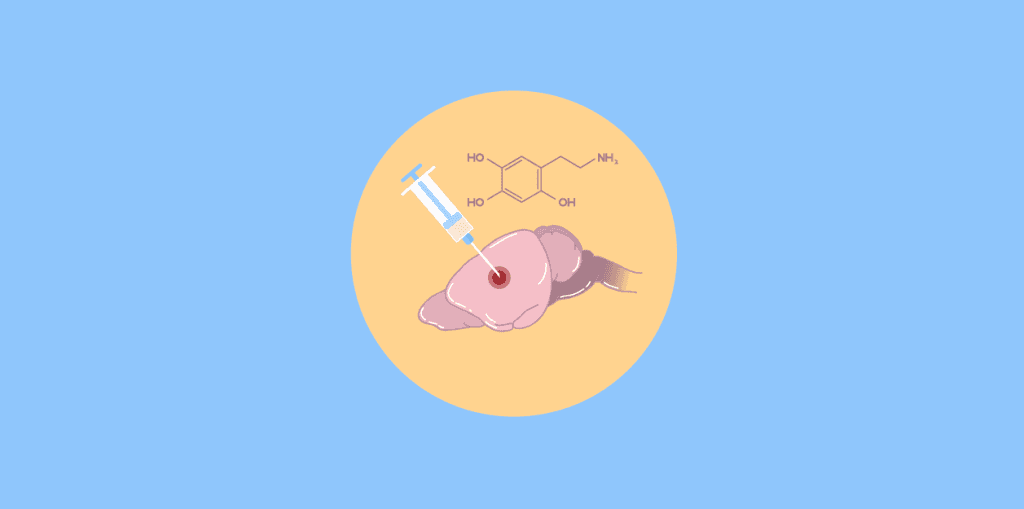
The 6-hydroxydopamine molecule is transported to the dopaminergic and noradrenergic neurons to cause degeneration of nerve terminals. 6-OHDA neurotoxicity is developed as it inhibits the mitochondrial respiratory enzymes (chain complexes I and IV). Due to the blockade of these enzymes, the neurons could no longer exert their normal physiological duties and consequently die. Since in Parkinson’s disease, the dopaminergic nigrostriatal pathway is mainly subjected to degeneration, so the animal models have been developed in which 6-OHDA induced lesions of the dopaminergic system are generated. Regional selectivity for the nigrostriatal tract could be achieved by injecting the toxin into different parts of the ascending nigrostriatal pathway. In the preclinical PD research, rat models have been widely used in which 6-OHDA was injected into either one of three target sites: substantia nigra pars compacta (SNc), medial forebrain bundle (MFB), or the caudate-putamen unit (CPu). It remains unclear, however, which of these models is most suitable for PD modeling. To model PD, the animal model must mimic both the degeneration of dopaminergic neurons and the behavioral deficits associated with idiopathic PD. 6-OHDA model has contributed enormously to enhance the understanding of PD pathology (Blesa., Phani., Jackson-Lewis., & Przedborski., 2012).
6-OHDA injection into the CPu
6-OHDA injection into the CPu results in more selective neuron damage in the nigrostriatal dopaminergic system. Following the injection, because of its retrograde transport to SN pars compacta (SNc), the nigral dopaminergic neurons undergo degeneration and apoptosis. In this animal model, usually dorsomedial and ventrolateral striatum are targeted. In rodents, the ventrolateral portion of the CPu receives signals from motor and sensorimotor areas of the neocortex, whereas its dopaminergic innervations project from the SNc. Whereas, the dorsal part of the CPu has a mixed DA innervation from both SN and ventral tegmental area (VTA), and receives inputs from the limbic system as well as from the frontal cortical areas making it equivalent to the nucleus caudatus in humans. Also, it shows remarkable effects on locomotion and drug-induced rotation behavior by lesioning the dorsomedial part of the CPu, whereas the injection of the neurotoxin into the ventrolateral parts provokes difficulties in movement initiation, skilled motor behavior, and sensorimotor orientation. Therefore, the lesions in rodent ventrolateral CPu resemble more closely the depletion of dopaminergic innervation in the putamen of PD patients.
6-OHDA injection in the MFB
6-OHDA injection into the MFB leads to almost total destruction of the dopaminergic neurons of the SNc projecting to striatum as well as of the VTA heading to the nucleus accumbens, eventually causing a postsynaptic denervation sensitivity of DA receptors. In response to the lesion-induced imbalance between the nigrostriatal systems in both hemispheres, the test animals show unilateral sensorimotor deficits enabling the researchers to evaluate the lesions and intensity of the neurotoxic effect by behavioral analysis. The most robust manifestation of this is spontaneous postural motor asymmetry, which causes the animals to rotate toward their impaired hemisphere. This could be increased by stress and in particular due to drugs- such as D1/D2 receptor agonist apomorphine or DA reuptake inhibitor d-amphetamine induced rotations. Whereas, the bilateral MFB lesion of the nigrostriatal system in adult animals causes severe sensorimotor impairment with rapid aphagia and adipsia. Nevertheless, the standard 6-OHDA rat model, generated by unilateral injection of 6-OHDA into the MFB is more pragmatic and permits a direct comparison of lesion effects and therapeutic regimens within a single test subject by the comparison of both hemispheres.
6-OHDA injection into the SNc (Deumens., Blokland., & Prickaerts., 2002)
To generate more selective PD model, the neurotoxin is injected into SNc to cause less dramatic damage in the dopaminergic system. In this model, the animals receive unilateral injection either medial and/or a single lateral injection. With SNc injection, almost 90% dopaminergic neuron loss could be achieved. The single lateral 6-OHDA injection spares the dopaminergic cells in the medial SNc and efficiently manifests a neuropathological finding of PD patients with dopaminergic innervation damage mainly within the lateral SN. Consequently, the dopaminergic fibers at the lesion side within the lateral CPu diminish dramatically as compared to the fibers at the medial parts of the caudate-putamen unit. Moreover, the remaining DAnergic innervation in CPu corresponds clearly to the degree of DAnergic cell depletion in SNc. One of the major limitations of this model is the small size of the injection site which could not lesion the adjacent structures, i.e., VTA and makes it a very challenging task; therefore, restricting its application to rare experimental designs.
6-OHDA neonatal injection
For bilateral degeneration of the DAnergic nigrostriatal pathway in neonatal rats, the neurotoxin solution is injected transcutaneously into lateral ventricles on postnatal day 1. Bregma, the anatomical landmark to define the correct coordinates, is visible in this developmental stage. This bilateral lesion surgery could not result in severe akinesia and sensorimotor deficits.
6-OHDA administration (Mercanti., Bazzu., & Giusti., 2012)
Post-operative care
Assessing the neuroprotective effects of the drug (Sedaghat., Roghani., & Khalili, 2014)
Modelling Parkinson’s disease (Blesa et al., 2012)
Parkinson’s disease could be efficiently modeled in laboratory animals using 6-OHDA neurotoxin that recreates specific pathological events and their behavioral outcomes. The development of PD animal models is valuable to test new neuroprotective agents and treatment strategies for PD. Parkinson’s disease is characterized by degeneration of dopaminergic neurons in the substantia nigra, loss of striatal DA fibers, and reduction of the striatal dopamine levels. Also, Lewy body formation is the most important neuropathological feature of PD. 6- hydroxydopamine (6-OHDA) is a powerful neurotoxin that selectively and rapidly destroys the catecholaminergic neurons. This model has been successfully applied to test preclinical therapies and new pharmacological and genetic therapeutic agents for Parkinson’s disease.
Assessment of the neuroprotective effect of Thymoquinone (Sedaghat., Roghani., & Khalili, 2014)
Parkinson’s disease (PD) is the most common neurological disorder with progressive degeneration of dopaminergic neurons for which only symptomatic treatments with no prevention of disease progression are available. This study was conducted to assess the neuroprotective effects of the Nigella sativa bioactive compound thymoquinone (TQ). The effects of TQ on behavioral and cellular abnormalities and oxidative stress markers were also assessed in the 6-OHDA experimental model of early PD in the rat. For this, the animals were treated with unilateral intrastriatal 6-hydroxydopamine (6-OHDA) injections with TQ. After 7 days, it was observed that apomorphine reduced the neurons on the left side of the substantia nigra pars compacta (SNC), and the malondialdehyde (MDA) and nitrite levels in midbrain homogenate were increased. While the activity of superoxide dismutase (SOD) was reduced in the 6-OHDA lesion group. It was also shown that the TQ pretreatment significantly improves turning behavior, prevents SNc neurons loss, and lowers MDA level. These results suggested that TQ possesses excellent neuroprotection against 6-OHDA neurotoxicity and could provide a beneficial treatment regimen for neurodegenerative disorders, including PD.
Analyzing the expression of Tgfβ1 and inflammatory markers (Haas., Zhou., & Spittau., 2016)
Parkinson’s disease (PD) is characterized by the complete loss of midbrain dopaminergic (mDA) neurons. Microglia-mediated neuroinflammation is a common hallmark of Parkinson’s disease and is believed to trigger the disease progression. 6-OHDA has been widely used to induce dopaminergic neuronal degeneration in rodents to mimic PD and to study neurodegeneration, neuroinflammation as well as therapeutic approaches for PD. In this study, the temporal and spatial expression patterns of anti-inflammatory and pro-inflammatory markers were analyzed in the 6-OHDA mouse model of PD. It was found that the activated microglia and neurons in the lesioned SNc and CPu express Transforming growth factor β1 (Tgfβ1). The data collected form this research presented an important role for Tgfβ1 as a lesion-associated factor that regulates microglial activation states in the 6-OHDA mouse model to prevent degeneration of uninjured neurons by releasing neurotoxic factors such as TNFα and nitric oxide (NO). This study validated the use of the 6-OHDA rat model for analyzing the expression levels of inflammatory markers involved in Parkinsonism.
Gene therapy (Hernandes-Baltazar et al., 2017)
The 6-OHDA PD model has also been used to demonstrate the neurotrophic therapy (NT). Neurotrophic therapy consists of directed gene delivery of neurotrophic factors such as brain-derived neurotrophic factor (BDNF), cerebral dopamine neurotrophic factor (CDNF), glial cell line-derived neurotrophic factor (GDNF), mesencephalic astrocyte-derived neurotrophic factor (MANF), and vascular endothelial growth factor (VEGF) through nanoparticles or viral gene vectors. The 6-OHDA model with neurotrophic therapeutic factors was used to prevent progressive neurodegeneration and to stimulate the functional regeneration of the nigrostriatal system. It was also studied that the recovery of dopaminergic neurons could improve motor function. It is therefore essential to identify further underlying mechanisms of oxidative stress, neurodegeneration, neuroinflammation, and neuronal death triggered by 6-OHDA. This knowledge is vital to discover novel therapies to treat Parkinson’s disease.