
Traditional academic publishing relies on static formats that flatten three-dimensional and dynamic data into text, images, and tables, limiting transparency, reproducibility, and accessibility. STL (stereolithography) files, the standard for 3D printing, offer a transformative alternative by enabling readers to rotate, measure, and physically reproduce the very models used in research. Case applications in anatomy, electrophysiology, procedural training, radiology, and surgical planning demonstrate how STL integration enhances comprehension, democratizes education, and anchors clinical rigor in the scholarly record. Technical challenges including licensing, metadata, hosting, workflow tools, and accessibility are real but surmountable, with solutions already emerging in the medical 3D printing community. Embedding STL models into publications shifts communication from passive observation to active exploration, strengthens reproducibility through direct data sharing, and expands equity by providing global access to high-fidelity resources. STL publishing is therefore not a technical luxury but an ethical and intellectual necessity, positioning academic communication for a future where knowledge is not only visible but tangible, testable, and shared.
For more than a century, academic publishing has been bound to static formats. The familiar PDF has served as a reliable archive, but it also represents a constraint by flattening complex, multidimensional data into text, images, and tables. This limitation is especially evident in medicine, where information is increasingly three-dimensional and dynamic. Radiologists routinely compress volumetric DICOM datasets into a handful of representative slices, while surgeons reduce intricate procedures into line diagrams. Even video files, though capable of capturing movement, remain one-directional and passive: they allow observation, not interaction [1].
Yet the practice of medicine itself has already outgrown these limitations. Across disciplines, three-dimensional data is becoming essential. Anatomical models, surgical guides, prosthetic design, electrophysiological mapping, and tissue engineering all rely on volumetric representations that cannot be adequately conveyed by static figures [1,2]. At the same time, the cost of 3D printing has fallen and the technology has matured, making it feasible for classrooms, laboratories, and hospitals to generate precise models on demand [2]. Still, the primary format of academic communication remains largely unchanged. A different future is already beginning to emerge. In 2014, GigaScience became one of the first journals to publish micro-CT datasets and associated STL files, embedding interactive model viewers alongside manuscripts and enabling readers to download or 3D-print scientific objects themselves [3]. In radiology, the Radiological Society of North America’s 3D Printing Special Interest Group has established consensus guidelines for image acquisition, segmentation, and STL export, explicitly recognizing printable models as clinically appropriate in a range of scenarios from congenital heart disease to craniofacial reconstruction [4]. And more recently, regulatory frameworks have begun to take shape: FDA-cleared software and quality-assurance standards now govern aspects of segmentation and model validation, signaling that STL-based workflows are moving from experimental to mainstream [5].
The implications for academic publishing are profound. Embedding STL files directly into research articles would allow readers to rotate, measure, and interrogate the very same models used by the authors. This transforms the reader from a passive observer into an active participant. It enhances transparency by exposing the underlying data, strengthens reproducibility by allowing independent validation, and expands accessibility by giving any student or clinician with a basic 3D printer the ability to hold in their hands what would otherwise exist only in text or images [1,6]. Academic publishing has always aspired to make knowledge public. By embracing STL integration, it can finally make knowledge tangible.
Publishing is built for text. It works when you’re reporting words, but it falls short when the subject is dimensional. PDFs lock volumetric or time-based data into a single frame. In medicine, that means something living and complex is reduced to a still image. Even in areas like surgical planning or prosthetic design, what should be interactive ends up frozen on a page [1].
Video and audio files were supposed to help, but they don’t solve the problem. A surgical video shows the motion but leaves the reader as a spectator. There’s no way to change the angle, slow it down in a meaningful way, or measure what you’re seeing. It’s one-way viewing, not exploration [1].
DICOM data show this limitation best. Radiology runs on three-dimensional datasets, yet journals almost never publish them in their full, navigable form. Instead, they collapse into a few 2D slices or compressed composites. This flattening strips away context, hides detail, and makes reproducibility almost impossible [4]. In conditions where subtle 3D relationships matter like congenital heart disease, craniofacial planning, and vascular anomalies, the difference between a slice and a model is the difference between understanding and guesswork. Even annotation systems don’t bridge the gap. Metadata can tag information but it can’t replace interactivity. The nuance of spatial and tactile understanding is lost. The irony is that the fields most dependent on depth like anatomy, electrophysiology, interventional medicine, and radiology, are also the ones most restricted by these static publishing norms. As others have noted, modern clinical science now depends on volumetric accuracy and validation, yet our publishing formats still flatten it [2,5].
STL, or stereolithography, is the standard digital format for 3D printing. It captures the surface geometry of an object in a way that makes it both explorable on screen and reproducible in physical form. For decades it has been the workhorse of engineering and design, but only recently has it begun to move into academic medicine [2]. One of the reasons STL is so powerful is its flexibility. Models can be opened in a simple browser-based viewer and rotated, zoomed, or annotated without any specialized software [3]. The same file can be sent to a 3D printer, giving students or clinicians a physical model they can hold, measure, or use in training [6]. Because STL is lightweight and widely compatible, it is already used across biomedical engineering, surgical planning, prosthetic design, and classroom teaching, and it is starting to appear in academic publishing as well [1,2]. This means that instead of flattening a structure into a single
figure, a researcher could publish the structure itself. A patella, for example, could be uploaded in STL format, allowing a reader not just to look at it but to rotate it, take measurements, or even print it for hands-on study.
Anatomy highlights how limited static formats have become. GigaScience began publishing STL files of micro-CT datasets to move beyond flat diagrams [3]. A patella in PDF is an outline; a patella in STL is an object to turn, inspect, and even hold. The ability to hold and examine accurate replicas of human anatomy enhances comprehension in ways traditional diagrams cannot [1]. Embedding STL models into articles transforms anatomy from memorization into exploration, ensuring that every student can interact with the same high-fidelity content.
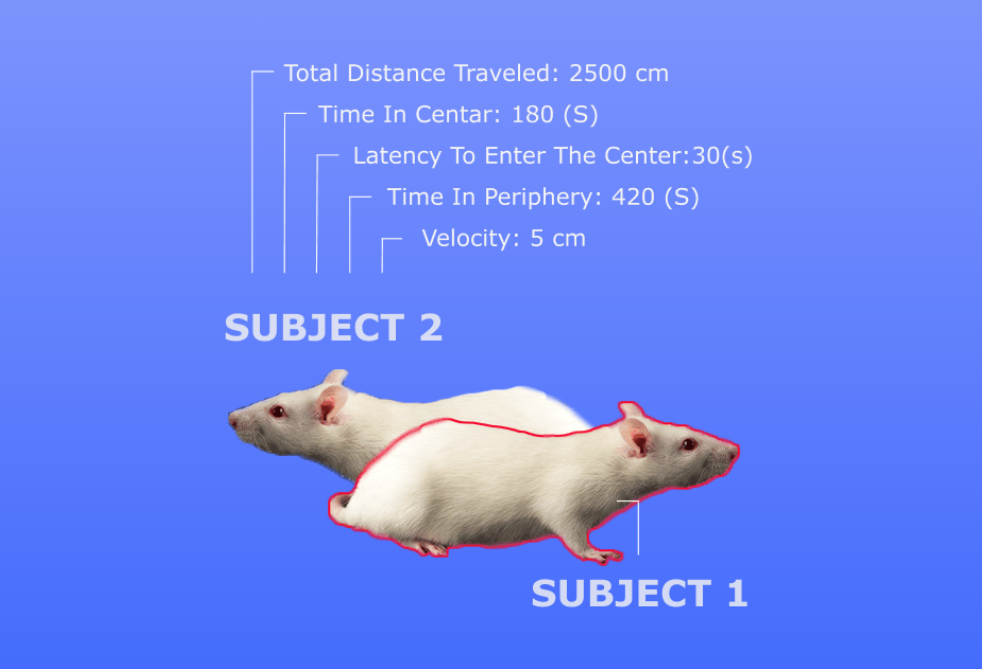
Electrophysiology underscores the same point in an even starker way. Conduction pathways are inherently three-dimensional, yet publications often flatten them into arrows on schematic maps.
Three-dimensional reconstructions are not optional when spatial relationships drive clinical interpretation [4]. Converting these data into STL-like meshes gives readers agency: they can rotate a pathway, zoom into branching circuits, and see dynamics that static figures cannot convey. Publishing in this way turns abstract electrophysiology into something tangible and reproducible, opening the field to broader participation and validation.
STL integration also democratizes procedural training. 3D-printed models have already been used to train clinicians in suturing, airway management, and vascular access, reducing training costs while expanding access to high-quality practice tools [1]. Extending this into publishing means a pericardiocentesis model, shared as an STL file, can be downloaded and printed by any trainee in the world. A single model, once published, becomes infinitely reproducible and infinitely teachable, making an impact that static diagrams or descriptions cannot match.
Procedural models further highlight the unique value of STL publishing. A low-cost, high- fidelity proximal interphalangeal dislocation model improved both perceived and observed competency among emergency medicine learners [7,8]. Earlier work on a low-cost pericardiocentesis trainer demonstrated how 3D printing could democratize access to rare, high-stakes procedures without reliance on cadavers or expensive simulators [7,8].
Radiology and surgery demonstrate how STL publishing could extend clinical rigor into research communication. RSNA guidelines affirmed the appropriateness of image-derived 3D models in conditions from congenital heart disease to craniofacial surgery [4]. These models already guide operative planning, helping surgeons anticipate complexity and improving outcomes. FDA-cleared segmentation software and formal quality assurance are now integrated into STL workflows, showing that reproducible, validated 3D data are already feasible [5]. Publishing STL outputs alongside radiology or surgical papers would embed clinical precision directly into the scientific record.
Across anatomy, electrophysiology, procedural training, and surgical planning, the pattern is clear. Static formats reduce dimensional data to images. STL publishing restores their depth, allowing readers not just to observe but to manipulate, measure, and replicate. The effect changes education, lowers barriers to training, and anchors reproducibility in a medium that matches the complexity of modern medicine.
Academic publishing has always been about more than recording knowledge. At its best, it is a vehicle for making science public, transparent, and reproducible. But the formats we rely on including text, images, and PDFs, no longer keep pace with the science itself. The question is now whether publishing can remain credible without them. Scientific communication is fundamentally strengthened by STL integration. Embedding STL files and interactive viewers into articles allows readers to rotate, zoom, and interrogate objects in real time [3]. Instead of trusting an author’s description, the reader engages directly with the data. This shift is transformative: communication becomes dialogic rather than declarative, empowering the reader to test, explore, and learn actively.
Education is elevated from abstraction to embodiment. The ability to hold and examine accurate replicas of human anatomy enhances comprehension in ways traditional diagrams cannot [1]. A diagram of a heart shows a silhouette; an STL model lets students look inside the atria, flip the orientation, and even 3D print a physical replica for hands-on practice. STL workflows make this process straightforward and scalable, meaning one published model can translate into thousands of classrooms worldwide [6]. Academic publishing then stops being a text to memorize and becomes an experience to inhabit.
Reproducibility and transparency are made possible, not just promised. FDA-cleared software and validation pipelines now exist for generating anatomical STL models [5]. When the STL file itself is published, the research community can confirm, replicate, or challenge findings directly. Appropriateness criteria issued for clinical scenarios where 3D models are indispensable underscore this imperative [4]. Embedding STL files into publications would make reproducibility a tangible reality rather than an aspirational buzzword.
Global accessibility transforms who can participate in science. 3D printing has already
democratized access to surgical planning, prosthetic design, and biomedical engineering by lowering cost and technical barriers [2]. The same is true in publishing. A medical student in a resource-limited setting, without access to cadavers or advanced imaging labs, can download a high-fidelity STL model and study the same anatomy as students in the world’s top medical schools. Knowledge that was once gated by geography and resources becomes equitably accessible.
Publishing is future-proofed by STL integration. Validated STL workflows are already being incorporated into AI, computer vision, and immersive AR/VR pipelines [5]. By embedding STL files into publications today, journals ensure their relevance in the data ecosystems of tomorrow.
The reproducibility demonstrated by low-cost models such as those developed by Lorde and colleagues shows that these benefits are already being realized across multiple institutions [7,8].
Taken together, STL integration is an ethical and intellectual necessity. Academic publishing
cannot claim transparency while omitting the very data that make findings reproducible. It
cannot claim accessibility while locking interactive knowledge behind static figures. And it
cannot claim to prepare science for the future while ignoring the formats on which that future depends. STL files matter because they return publishing to its highest purpose: to make knowledge not only visible, but usable, testable, and shared.
The promise of STL publishing is clear, but integrating three-dimensional models into the
scholarly record requires addressing several practical challenges. Far from diminishing the case, these obstacles clarify the standards and infrastructure needed to make STL publishing viable. Licensing and copyright are the first hurdle. STL files sit at the intersection of data and design. Should a patient-specific anatomical model be treated as raw scientific data, freely shareable under Creative Commons? Or is it an intellectual property product of the institution or surgeon who created it? Without clear frameworks, uncertainty around ownership may discourage authors from publishing their models at all, while excessively restrictive licenses limit reuse and validation, undercutting the very purpose of publishing [4]. Striking the right balance by encouraging openness while protecting sensitive data is central to the credibility and adoption of STL publishing.
Metadata and hosting are equally critical. An STL file without context is an orphan. Meaningful sharing requires robust metadata describing not just geometry, but also the methods of segmentation, resolution, smoothing, anonymization, and intended use [5]. Without this, readers cannot judge quality or replicate the process. Permanent hosting is another challenge: a file attached to a supplementary folder is vulnerable to link rot. Long-term repositories such as the NIH 3D Print Exchange or journal-integrated viewers offer stability, but journals must commit to infrastructure that ensures files remain accessible years after publication. Without permanence, reproducibility becomes impossible.
Software and workflow tools form the technical backbone. Fortunately, the ecosystem already exists. Open-source platforms such as 3D Slicer support segmentation and STL export from DICOM, while OsiriX/Horos are widely used in radiology. Web-based mesh viewers like Sketchfab or custom journal integrations make models explorable directly in the browser, but adoption and standardization remain the bottleneck [4,6]. Training researchers to use these platforms consistently, and requiring journals to set minimum technical standards, will ensure that STL publishing maintains scientific rigor.
File size and accessibility remain practical but non-trivial issues. STL models can be large, especially when derived from high-resolution CT or MRI scans. Without compression or
streaming, downloading becomes prohibitive for readers in bandwidth-limited environments. Optimized file formats and delivery systems are essential to ensure STL publishing does not widen the digital divide [2]. The same technology meant to democratize access could inadvertently reinforce inequity if not carefully managed.
Taken together, these challenges should not be viewed as reasons for hesitation but as roadmaps for action. Licensing, metadata, software, and accessibility have solutions already emerging in the medical 3D printing community. Addressing them systematically will allow STL publishing to move beyond early demonstration projects and become the standard for how dimensional science is communicated, validated, and preserved.
For STL publishing to become routine, researchers need a clear and reproducible workflow. The process builds on tools already familiar to radiologists, engineers, and biomedical scientists, but it must be standardized to ensure consistency and scientific integrity.
Source Data
STL models begin with primary datasets. In medicine, these are most often DICOM imaging studies such as CT or MRI scans; in biology, microscopy volumes; and in engineering, direct
CAD outputs. High-quality source data determine the fidelity of the final model [6]. Publishing the STL without citing its origin is meaningless; the model is only as credible as the data it represents.
Segmentation and Processing
Raw images require careful segmentation and cleaning to separate structures of interest and remove noise. Open-source software such as 3D Slicer, or radiology platforms like OsiriX and Horos, support this workflow. The importance of producing watertight geometry and eliminating artifacts must be stressed because noting that poorly processed models can mislead more than they educate [4]. Standardized segmentation protocols and their explicit documentation are therefore essential for reproducibility.
Export to STL
Most imaging and modeling platforms allow direct export to STL format. Resolution must be balanced against file size: overly high-resolution models can become unwieldy, while excessive simplification sacrifices accuracy. One could successfully accomplish this by choosing the highest fidelity consistent with feasible sharing and printing [4].
Optimization for Publication Before dissemination, models should be optimized for clarity and accessibility. This includes mesh simplification to reduce file size, anonymization to remove protected patient information, and normalization of orientation and scale. Attaching metadata including segmentation methods, resolution, and licensing terms, ensures that published models are not just files but citable, reusable research objects [5].
Hosting and Visualization
STL files require stable, long-term hosting and user-friendly viewing. Journals may choose to embed lightweight viewers directly into manuscripts [3], or deposit files in repositories such as the NIH 3D Print Exchange or institutional servers. What matters most is permanence and accessibility because without it, STL publishing loses its value.
Citation and Sharing
STL models should be treated as primary research outputs. Assigning DOIs, citing segmentation methods in the methods section, and clarifying licensing terms such as Creative Commons, transforms STL files from supplementary “extras” into legitimate, traceable components of the scholarly record [4]. Together, these steps establish a reproducible pipeline that is already feasible with current infrastructure. What is needed now is not new technology but consistent adoption and enforcement by journals. Once standardized, STL publishing will integrate seamlessly into the research ecosystem, allowing dimensional data to be shared, validated, and built upon as naturally as text and figures [4].
What matters next is how journals turn static articles into living environments for learning, validation, and discovery. When an STL model enters an AR or VR headset, anatomy stops being a picture and becomes a place. Trainees can step around a structure, inspect a corridor of bone, or practice a trajectory before they touch a real patient. This is not speculative. The same 3D printing ecosystem that already supports surgical planning and biomedical design can feed immersive training with the very models authors publish [2]. The path is simple: publish the STL, render it in a browser, and allow optional export to AR or VR viewers. One model, three learning modes.
Models are training data for AI and computer vision. STL files give machine learning pipelines clean surfaces, explicit geometry, and reproducible provenance. That is exactly what modern validation requires. With FDA-cleared segmentation tools and quality programs now standard in clinical modeling, the output is ready for benchmarking and reuse rather than locked inside screenshots [5]. The more journals publish models with methods, the faster the field can build shared datasets for algorithm development and head-to-head comparisons.
Reviewers should not be guessing from a figure. They should rotate the model, measure a margin, and verify that the segmentation matches the stated method. Publishing the STL with clear metadata, licensing, and a persistent identifier turns peer review into a direct interactive examination rather than an inference exercise [4,5]. Versioned models with change logs make post-publication updates transparent and citable.
A single STL model can become a thousand classrooms. Anatomy, procedure rehearsal, and
device design all change when an article ships with a printable object. Students who lack cadavers or high-cost simulators can still learn on high-fidelity models that match the paper exactly, closing the gap between wealthy and resource-limited settings rather than widening it [1,2,6]. Dr. Spencer Lord’s work illustrates this principle in practice: his 3D-printed
pericardiocentesis and joint reduction models showed that low-cost, reproducible tools can improve learner performance and be shared across institutions [7,8]. These are teaching aids but also evidence that STL files published with research can scale into global training resources. When the model is part of the article, every learner has the chance to print the same object, rehearse the same procedure, and build competency on equal terms. Taken together, these directions point to a single outcome. Publishing will act as a portal to the data and the experience that produced the conclusions.
STL files change what it means to publish. When the model is present, readers do not trust a description. They test the object. They turn it, measure it, print it, and learn from it. That is real transparency. That is reproducibility you can hold. Medicine already runs on three-dimensional understanding. Radiology, surgery, and education depend on geometry, not just prose. The RSNA 3D Printing SIG has formalized clinical appropriateness and workflow standards. Regulatory guidance and FDA-cleared tools have matured the pipeline from imaging to validated interactive, in browser, practical models [3-5]. The ethical case is just as strong. If we claim to share knowledge, we should share the thing itself, not only a picture of it. If we claim to support equity, we should let a student anywhere in the world download the same model that trained the author. If we claim to value reproducibility, we should publish the artifact that makes replication possible [1,2,6]. STL is the difference between reading about a result and interrogating it. Academic publishing has always aspired to make knowledge public. With STL files, it can make knowledge tangible and testable, and it can align the scholarly record with the way modern medicine actually works [3-5].
1. Ventola, C. L. (2014). Medical applications for 3D printing: Current and projected uses.
P & T, 39(10), 704–711. PMID: 25336867; PMCID: PMC4189697.
2. Bozkurt, Y., & Karayel, E. (2021). 3D printing technology; methods, biomedical applications, future opportunities and trends. Journal of Materials Research and Technology, 14, 1430–1450. https://doi.org/10.1016/j.jmrt.2021.07.050.
3. Edmunds, S. (2021, March 9). A step-by-step guide to 3D print a scientific publication.
GigaScience Blog.Retrieved from https://gigasciencejournal.com/blog/a-step-by-step-
guide-to-3d-print-a-scientific-publication/.
4. Chepelev, L., Wake, N., Ryan, J., Althobaity, W., Gupta, A., Arribas, E., … Rybicki, F. J. (2018). Radiological Society of North America (RSNA) 3D Printing Special Interest Group (SIG): Guidelines for medical 3D printing and appropriateness for clinical scenarios. 3D Printing in Medicine, 4(1), Article 11. https://doi.org/10.1186/s4125-018- 0030-y.
5. Paxton, N. C. (2023). Navigating the intersection of 3D printing, software regulation and quality control for point-of-care manufacturing of personalized anatomical models. 3D
Printing in Medicine, 9(9), 1–12. https://doi.org/10.1186/s41205-023-00175-x.
6. Pamidi, A. S., Spano, M. B., & Weiss, G. A. (2024). A practical guide to 3D printing for chemistry and biology laboratories. Current Protocols, 4(10), e70036.
https://doi.org/10.1002/cpz1.70036.
7. Lord S, Lord G, Geary S. A novel, low-cost, low-fidelity pericardiocentesis teaching
model. West J Emerg Med. 2021;22(4):931-936. doi:10.5811/westjem.2021.3.49876
8. Lord S, Lord G, Geary S. Application of a low-cost, high-fidelity proximal phalangeal
dislocation reduction model for clinician training. West J Emerg Med. 2023;24(5):839-
846. doi:10.5811/westjem.59471
Written by researchers, for researchers — powered by Conduct Science.








Is a transitional year resident physician pursuing a career in diagnostic neuroradiology with a background in biochemistry. She is the founder of a collaborative initiative focused on radiology, artificial intelligence, and deep learning, connecting students and physicians through shared opportunities, interdisciplinary research, and mentorship. Beyond her research, she explores the integration of creative technologies such as virtual reality and 3D modeling into medical education and clinical practice. A VR enthusiast and artist, she believes that creativity and compassion should remain at the heart of patient care.
