

Real-world evidence is essential in medical research. Real-world data has numerous benefits over randomized controlled trials, particularly in studying Parkinson’s disease. In fact, Parkinson’s is one of the most prevalent neurodegenerative diseases worldwide, with no current treatments being able to cure the disease. Only in the US, there are more than 630,000 people affected by this condition (Tanguy, Jonsson & Ishihara, 2017).
Since managing Parkinson’s disease can be challenging, with symptoms fluctuating daily and between patients, collecting health-related data in real time is vital. Note that real-world data is defined as medical information collected in non-experimental environments. Sources vary from administrative claims to social media channels. Data across real-life settings and diverse populations can provide valuable insights into disease progression, natural history of the disease, treatment programs, and socioeconomic burdens. It can reveal important aspects of the daily lives of people with Parkinson’s disease and the effectiveness of novel treatments. Consequently, longitudinal real-world data can improve interoperability, Parkinson’s disease management, and financial decisions.
Research in the field of oncology is sensitive and challenging. Note that there are various cancer treatments, with radiation therapy and chemotherapy being among the most common interventions (“Types of Cancer Treatments,” 2017). With the increasing use of digital health solutions and experimental cancer therapies, though, real-world data can support numerous aspects of medical research and routine clinical practice. Some of its applications include:
Parkinson’s disease is a complicated medical condition, defined as a central nervous system disorder. The wide range of symptoms and complications requires the use of different measurements for the effective management of the disease. Interestingly, a recent literature review explored the benefits of various Parkinson’s disease measurements, classified into the following dimensions of assessment (Tanguy, Jonsson & Ishihara, 2017).
Yet, this research classification should be further harmonized across local and international research and administrative bodies.
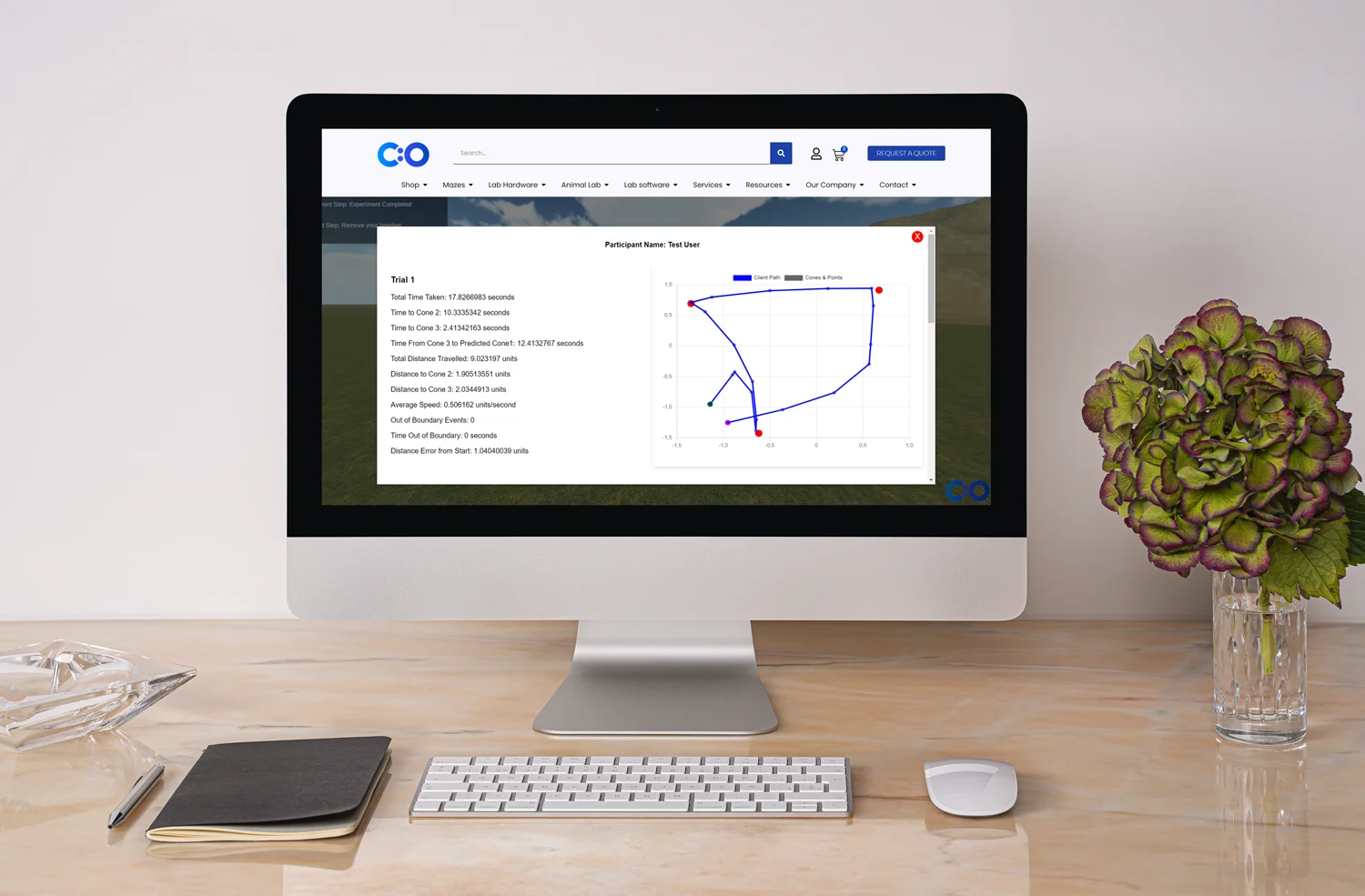
Parkinson’s is a progressive neurogenerative disease with severe complications. Since symptoms fluctuate on a daily basis and between patients, real-world data is needed to measure symptoms, assess treatments, benefit financial decisions, and improve patients’ quality of life. Note that a recent study showed that smartphone assessments could provide valuable clinical insights, including frequent real-world data (Zhan et al., 2018). Zhan and colleagues assessed 129 Parkinson’s patients who completed five tasks on a mobile app. The tasks measured finger tapping, balance, gait, voice, and reaction time, providing data from 6,148 smartphone activity assessments in total. mHealth apps can help patients with chronic conditions track their symptoms, manage medications, store insurance information, and find social support. Practice shows that mobile sensors which track symptoms and Parkinson’s apps which show exercises (e.g., to improve balance and posture) are highly beneficial well-being. What’s more, Parkinson’s disease research shows that real-world measurements and remote monitoring can reduce research costs and improve health outcomes. Data collection in real time complements scientific findings: it provides vital information that annual medical visits are unable to capture. Last but not least, the mHealth approach in medicine is growing in popularity as it empowers and motivates patients. A recent initiative revealed that patients with Parkinson’s disease are willing to share their health-related data to contribute to research and routine clinical practice. Interestingly, 4,218 people from more than 50 countries provided a large source of medical information, including symptoms scores, patient-reported outcomes surveys, diary entries, and data from patients’ wearables.
With the transfer of medical information into electronic datasets, electronic health records and administrative claims also reveal some impressive benefits over standard clinical trials. In fact, although randomized controlled trials are still the gold standard in research, real-world data is vital. It can address some of the major obstacles in Parkinson’s disease research, such as strict inclusion criteria, poor generalizability, underrepresented populations, high costs, unexpected delays, and a lack of follow-up information (especially in non-pharmacological interventions). Medical claims databases, on the other hand, offer some impressive advantages over standard trials (Bloem et al., 2018). Administrative claims provide information about diverse populations, real-world settings, and co-morbid conditions. Investigating a medical claims dataset is more cost-effective than traditional clinical trials. Electronic health records also provide robust real-world data, including medical history and prescriptions, which can complement scientific findings.
In conclusion, real-world data plays an important role in research and practice. When it comes to Parkinson’s disease research, longitudinal real-world data benefit the evaluation of epidemiology, treatment management, and payment decisions. Parkinson’s disease, as explained above, is one of the most challenging neurological diseases, which affects millions of people worldwide. Since researchers and practitioners cannot capture all the varying symptoms and side effects associated with the disease, interventions are often individualized. Hence, longitudinal real-world data is essential to complement medical findings and improve clinical decisions.
With the increasing capabilities of today’s digital health solutions, electronic sources of real-world data are becoming more and more popular. Sources, such as administrative claims and mHealth apps, support data collection, and analysis across various domains of research (e.g., cognition, quality of life, etc.). Note that digital solutions facilitate data collection, increase user engagement, and empower patients. In the end, real-world evidence is reshaping the future of Parkinson’s research – improving patients’ health outcomes and quality of life.
Bloem, B., Ypinga, J., Willis, A., Canning, C., Barker, R., Munneke, M., & De Vriesa, N. (2018). Using Medical Claims Analyses to Understand Interventions for Parkinson Patients. Journal of Parkinson’s Disease, 8(1), p.45-58.
Lee, S., Kim, S., Cheon, S., Seo, J., Kim, M., & Kim, J. (2016). Activities of daily living questionnaire from patients’ perspectives in Parkinson’s disease: a cross-sectional study. BMC Neurology.
Merola, A., Romagnolo, A., Rosso, M., Suri, R., Berndt, Z., Maule, S., Lopiano, L., & Espay, A. (2018). Autonomic dysfunction in Parkinson’s disease: A prospective cohort study. Movement Disorders, 33(3), p. 391-397
Opara, J., Brola, W., Leonardi, M., & Blaszczyk, B. (2012). Quality of life in Parkinson`s Disease. Journal of Medicine and Life, 5(4), p. 375-381.
Opara, J., Malecki, A., Malecka, E., & Socha, T. (2017). Motor assessment in Parkinson`s disease. Annals of Agricultural and Environmental Medicine, 24(3), p. 411-415.
Romann, A., Dornelles, S., Maineri, N., Rieder, C., & Olchik, M. (2012). Cognitive assessment instruments in Parkinson’s disease patients undergoing deep brain stimulation. Dementia & Neuropsychologia.
Sleep disorders in Parkinson’s disease: Diagnosis and management (2011). Annals of Indian Academy of Neurology.
Tanguy, A., Jonsson, L., & Ishihara, L. (2017). Inventory of real-world data sources in Parkinson’s disease. BMC Neurology.
Zhan A, Mohan S, Tarolli C, Schneider R, Adams J, Sharma S, Elson M, Spear K, Glidden A, Little M, Terzis A, Dorsey E, Saria S. (2018). Using Smartphones and Machine Learning to Quantify Parkinson Disease Severity The Mobile Parkinson Disease Score. JAMA Neurol, 75(7), p.876-880.







Shuhan He, MD is a dual-board certified physician with expertise in Emergency Medicine and Clinical Informatics. Dr. He works at the Laboratory of Computer Science, clinically in the Department of Emergency Medicine and Instructor of Medicine at Harvard Medical School. He serves as the Program Director of Healthcare Data Analytics at MGHIHP. Dr. He has interests at the intersection of acute care and computer science, utilizing algorithmic approaches to systems with a focus on large actionable data and Bayesian interpretation. Committed to making a positive impact in the field of healthcare through the use of cutting-edge technology and data analytics.
