

Digital health research plays a crucial role in telemedicine and e-health, which can be defined as medical treatment and research delivered by technology.
Digital health research is much more than data collection, remote observation, and increased mobility. In fact, digital health research empowers patients, provides personalized care, and benefits connected care pathways (“mHealth… What Does It Really Mean?” 2014). It isn’t only about apps and technology solutions. Digital health research represents a whole shift in ideas: patients become active participants in research and practice.
With the implementation of digital health research solutions, research institutions and stakeholders have started to adopt patient-centered care to catch up with today’s healthcare demands. In fact, numerous studies reveal the perceived potential of digital health research and mHealth. For instance, an international study conducted across the USA, China, Brazil, and India (Kayyali et al., 2017) showed that 89% of healthcare practitioners, 75% of patients, and 73% of users, believe that digital health research and mHealth can improve real-life outcomes.
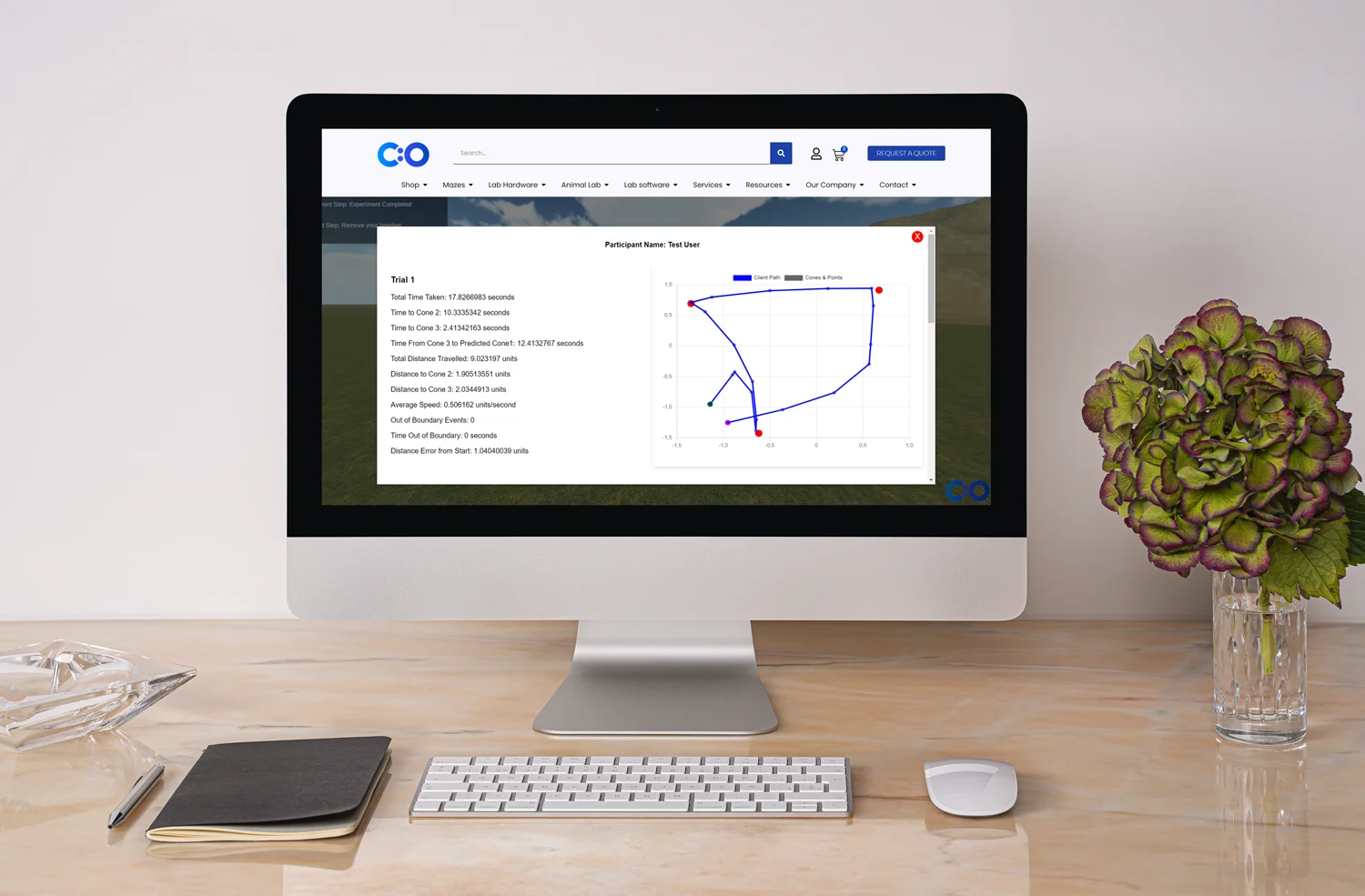
Digital health research is popular among users as it involves the usage of mobile devices. As mHealth is supported by the wide use of mobile tools, researchers also benefit from technology. The impressive computing and communication capabilities, such as text messages and GPS, facilitate data collection, management, analysis, and communication. Not surprisingly, mobile devices have replaced personal digital assistants (PDAs) and pagers. With their advanced features, such as maps, high-resolution screens, powerful operating systems, and compact sizes, mobile devices and smartphones, in particular, are more user-friendly, accessible, and effective (Ventola, 2014).
To sum up, the use of mobile devices gives researchers access to:
Mobile devices support the increase in popularity and effectiveness of digital health research. So do apps. Health apps are medical software programs designed to run on a mobile device and accomplish a certain goal (Ventola, 2014).
From studying diabetes to fitness, health apps offer an interactive way to reach participants and provide a systematized approach to data management. The only thing people need to do is download an app. On top of that, cloud computing offers numerous data storage options, which guarantee safety. Note that consent forms are also being integrated into app-based research. Thus, researchers can forget about time-consuming paperwork, medical records, and additional output, and participants can be sure that their data is safe and confidential.
Achieving meaningful results to improve patient’s lives has always been the main objective of the research. In fact, patients’ well-being is the main reason why digital health research solutions broaden research and benefit medical findings. Neurological, cognitive, biological and even environmental studies can only gain from technology. Not surprisingly, researchers use apps as they have realized the advantages of mobile devices and applications. By implementing technology into healthcare, medical professionals, programmers and patients work together towards the future of medicine.
As clinical trials play a crucial role in research, digital health research can only benefit studies (“Software-enabled clinical trials,” 2017). More and more companies implement technology into practice and move to digital data. Virtual trials (conducted outside of the hospital) and digital biomarkers (sensors and wearables) are popular among experts. With tech and interoperability innovations, digital health research leads to effective recruitment, cost-effective methods, rich data, and meaningful analyses.
Digital health research is powerful. However, researchers need to consider some vital aspects when initiating app-based research and digital clinical trials:
Design: Designing research is a long process and developing an app adds some additional demands to the study. Data shows that the average time for creating an app is about 18 weeks. Note that user testing with real end-users is crucial. Testing includes usability testing, and usability inquiries. Usually, usability testing evaluates interfaces and protocols. On the other hand, usability inquiries include surveys and interviews to assess users’ experiences and needs.
Usability: When designing an app, researchers and sponsors need to focus on design and usability. Having more usable applications will foster engagement and motivation (Zapata, 2015). Research shows that to be successful, apps must be easy to use. In fact, usability is defined as the facility people can use a technological tool to perform a task and achieve a goal. Usability can determine research success. According to the ISO/IEC9126–1 quality model usability involves understandability, learnability, operability, and attractiveness. These aspects aim to achieve efficiency, effectiveness, and satisfaction. For instance, users report that the color black and small letters are not attractive. Experts need to consider the fact that elderly users are not interested in gaming apps and younger adults perform online tasks faster. Programmers need to understand that a monotonous interface and too much text decrease learnability and efficiency. Difficulty in scrolling and navigating menus also need to be considered.
Reminders: In fact, talking about designs and usability, it’s been proven that push notifications facilitate clinical trials, research, and treatment. By integrating reminders in an app, experts can engage users and help them manage their drug intake better, for example. Of course, reminders should not be invasive.
Relevance: Creating a health app might be exciting, but programmers, patients, and medical professionals need to work together to create a relevant app. Users should not be presented with confusing apps, experts should not be overwhelmed with complex analytics, and healthcare providers should not experience technology fatigue in their already stressful working environment. In other words, additional administrative and technology burdens should be avoided.
Mobility: When it comes to digital health research, experts need to take advantage of the mobility aspect related to digital health research. Smartphones take patients away from clinics and labs. What’s more, technology can connect devices, solutions, and institutions and improve practices (“mHealth…What does it really mean?” 2014).
Time & Costs: The development of a health app needs to be relevant and effective. That means that technology should reduce doctor’s visits, interventions, and readmissions. Data should be used effectively to reduce costs. In fact, when it comes to digital recruiting, data shows that virtual trials can cost half as much compared to a traditional on-site study (“Software-enabled clinical trials,” 2017).
Safety: Technology connects systems, scenarios, and institutions. As technology solutions provide real-time updates from a wide range of inputs, safety needs to be considered. Note that stakeholders also need to have access to information, which should be confidential and secure. Data exchange needs to be supported by protocols, consent forms, and safe cloud platforms.
Personal Characteristics: Most of all, healthcare technologies should focus on patients. Personal characteristics, such as age and education, need to be considered. It’s interesting to mention that a study on diabetes showed that people felt the need of social interactions, chat rooms, and forums (Kayyali et al., 2017). What’s more, each topic of research requires different study methods and approaches, so apps need to be personalized and efficient.
The topic of digital health research is gaining more and more popularity. Telemedicine and mHealth are becoming an everyday practice for trials, research, and treatment. Digital health research solutions are widely used, and the number of companies and institutions that implement technology into practice is increasing (“Software-enabled clinical trials,” 2017). That’s not surprising. Smartphones and apps are popular among users – with fitness and nutrition apps being on the rise. To answer users’ demands, interactive designs should follow the main principle of usability. Therefore, visual functions, such as graphs, videos, and games, need to be incorporated without decreasing the levels of learnability and understanding.
To sum up, the main purpose of digital health research in research is to improve patients’ well-being. Technology makes businesses more competitive – all with a focus on consumers. Patients are active participants who have access to information and who use personal and sophisticated tools to manage their conditions. Most of all, digital health research aims to make healthcare accessible and affordable – regardless of age, background, and location (“mHealth…What does it really mean?” 2014).
Digital health research is not a futuristic theme in a sci-fi film: it’s a real shift in medical practices worldwide. Digital health research has created a whole new ecosystem; an ecosystem where stakeholders, researchers, healthcare experts, and patients work together to improve people’s health and well-being.
Kayyali, R., Peletidi, A., Ismail, M., Hashim, Z., Bandeira, P., & Bonnah, J. (2017). Awareness and Use of mHealth Apps: A Study from England. Pharmacy (Basel), 5 (2).
mHealth… What Does It Really Mean? (2014). The Journal of mHealth, 1 (2).
Software-Enabled Clinical Trials (September 4, 2017). Retrieved from https://blog.andreacoravos.com/software-enabled-clinical-trials-8da53f4cd271
Ventola, C. (2014). Mobile Devices and Apps for Health Care Professionals: Uses and Benefits. Pharmacy & Therapeutics, 39 (5).
Zapata, B., Fernandez-Aleman, J., Idri, A., & Toval (2015). Empirical Studies on Usability of mHealth Apps: A Systematic Literature Review. Journal of Medical Systems, 39 (2).







Shuhan He, MD is a dual-board certified physician with expertise in Emergency Medicine and Clinical Informatics. Dr. He works at the Laboratory of Computer Science, clinically in the Department of Emergency Medicine and Instructor of Medicine at Harvard Medical School. He serves as the Program Director of Healthcare Data Analytics at MGHIHP. Dr. He has interests at the intersection of acute care and computer science, utilizing algorithmic approaches to systems with a focus on large actionable data and Bayesian interpretation. Committed to making a positive impact in the field of healthcare through the use of cutting-edge technology and data analytics.
