

Advanced digital technology has become an integrated part of today’s health care industry. With the increasing use of smartphones worldwide, mHealth app development has become an essential aspect of digital health. Note that mHealth apps are defined as software programs for a mobile device designed to improve patient health outcomes. Figures show there are more than 325,000 health apps available online, which can be divided into higher-risk apps and lower-risk apps (Van Velthoven et al., 2018). Interestingly, wellness and chronic disease management apps are the top two categories that reveal high user engagement, retention, and satisfaction.
Yet, despite the popularity of mHealth apps, users, providers, and regulatory bodies agree that app development can face numerous challenges. Note that the process of mHealth app development covers various steps, such as planning, research, design, and testing. One of the major challenges consists in the fact that apps can be developed quickly by people with non-medical experience. As a result, some apps may lead to poor content, low-quality care, and negative outcomes. With the increasing use of apps among patients and clinicians, the lack of evidence-based principles for app development can result in deterioration in health.
Therefore, standards and strict guidelines are needed to ensure consistency and patient well-being. To create effective standards for innovative technologies, health software developers must review multidisciplinary standards, such as the ISO 14971:2007 Application of Risk Management to Medical Devices and the International Society for Pharmaceutical Engineering (ISPE) Good Automated Manufacturing.
Standards for mHealth app development: With a large number of health apps available online (paid and free) and more than 45,000 mHealth app developers (Kao & Liebovitz, 2017), health app development faces numerous challenges. A recent systematic review revealed that there are no clear regulations for the development of mHealth programs (Van Velthoven et al., 2018). Standards, as explained earlier, are essential to reduce risks, boost revenue, and improve access and quality. Depending on their various functions and purposes, health apps must be strictly regulated to improve patient outcomes and safety. Standards can also enhance a company’s reputation and benefit economies. At the same time, regulatory oversight should not become a burden to technological advancement, which is developing at a rapid pace. Thus, one of the most effective ways to improve innovative regulations concerning mHealth app development is an open crowd-sourced app rating system. Such a system can be used to validate standards; it can help experts examine app content and allow consumers to rate app usability. Scientific evidence is also crucial to enhance the standardization of mHealth app development. In fact, more and more randomized controlled trials and literature sources support the rapid pace with which mHealth app development is expanding. Note that clinical trials and publication practices might be time-consuming, so real-world evidence is essential in research.
Privacy concerns in mHealth app development: Healthcare app developers should also consider patients’ privacy and safety. Medical information is sensitive, and personal health information management can be a tricky task. It’s not a secret that health apps require confidential details, such as name, age, and access to stored data. Such data should not be used without consent; boxes that grant permission must be implemented. App developers have faced strong negative reactions after some companies have used data without approval. Cloud adoption is another major challenge for developers. Note that since some cloud-based storage databases cannot be properly secured, innovative standards and security regulations must be employed in app development practices (Van Velthoven et al., 2018).
Hospital information systems and mHealth app development: Since mHealth apps collect a wide range of metrics and personal information, data can be integrated into hospital information systems and electronic health records (EHRs). Nevertheless, app developers must decide which information is valid in order to be integrated into patients’ medical records. Mathematical algorithms and clear standards can facilitate app development. To set an example, the Substitutable Medical Applications and Reusable Technologies (SMART) is an innovative initiative which can help developers create apps that run across various electronic health records platforms. Note that SMART employs the Fast Healthcare Interoperability Resources (FHIR), which is a draft standard for exchanging digital health records. Interestingly, companies like Epic allow developers to access their electronic health records system. Free and easy access can also help patients and providers track appointments and check test results. Personal health records (PHRs) kept by the patients – not the providers – are also essential in today’s app development. Such tools can help users store medical information (e.g., blood type) across multiple networks and beyond borders (Kao & Liebovitz, 2017).
Benefits of mHealth app development: Although app development is a challenging area, mHealth app developers can create health apps with multiple benefits, for both patients and providers. Health care apps and e-patient portal apps can facilitate communication and research. Health professionals can prescribe apps and wearables to track treatment and medication adherence. With sophisticated audio and video capabilities, mobile devices and programs can help people with disabilities or users in remote locations access medical care. In addition, apps can boost a company’s revenue and reputation.
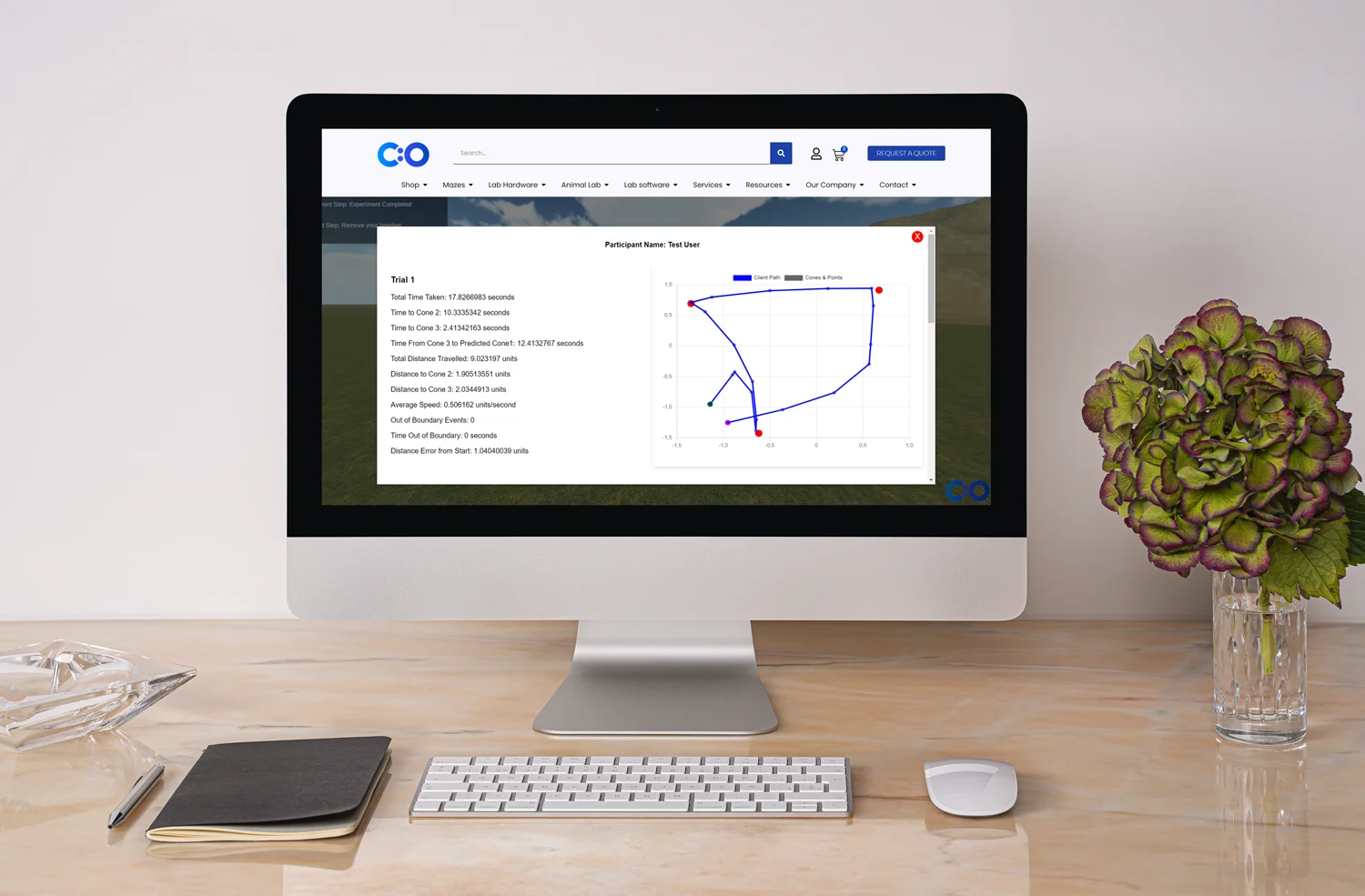
mHealth app development explained: Thus, the number of app developers is increasing. Developers can create apps from scratch for Android, iOS, and Windows operating systems. Note that previously, app developers have been criticized for creating high-end apps only for certain operating systems (e.g., Android). Application programming interfaces (APIs) can benefit app development, so different apps will meet different user needs (e.g., review prescription). The successful integration of artificial intelligence and machine learning is an essential factor for success in the field of mHealth app development. Nevertheless, as explained earlier, strict guidance is needed to support the process. We should mention that some apps have been taken down for promoting unhealthy choices (e.g., pro-smoking apps). The Food and Drug Administration (FDA) regulations are also needed to help providers and consumer choose a health app, which can improve patients’ well-being.
Areas of mHealth app development: Some of the most prominent areas of app development include wellness management, disease management, medication compliance, and self-diagnosis (Kao & Liebovitz, 2017):
In today’s tech-driven world, it’s not surprising that the health care industry has turned to digital solutions to support patients, increase revenue, and improve research. Smart devices and BYOD approaches become major game-changers. Digital solutions can provide various services, such as online consultation, self-diagnosis, and wellness management programs. mHealth apps, in particular, allow patients to access medical data, track medication intake, and contact health care providers in real-time, without being admitted to the hospital. Health apps help users organize and store their medical and financial details, as well as synchronize their personal data across platforms and digital formats worldwide. In addition, mHealth apps can be utilized to access information regarding medical results, prescribed medications, and support groups.
Nevertheless, health app development is facing numerous challenges. One of the major goals is global compliance with privacy regulations and clear standards, such as the Health Insurance Portability and Accountability Act (HIPAA) rules. At the same time, the compliant app development process can become limiting; it forces developers to create a health app based on strict regulations, which might fall behind digital innovations and creativity. Therefore, app developers must find a balance between regulatory standards and innovative technologies to boost patient health outcomes and well-being (Van Velthoven et al., 2018). Note that mHealth apps have the potential to improve a wide range of health-related aspects, such as wellness management, disease management, self-diagnosis, and mental health. The health information that apps collect can be integrated into patients’ records across countries in order to support interoperability and medical research.
To sum up, technology has become an integrated part of health care, with mHealth app development transforming the future of medical research and routine clinical care. With the increasing use of smart devices, patients and providers rely on health apps to facilitate diagnosis, treatment, and care. Hence, app developers should work along with regulatory bodies, health professionals, and users to create original and effective mHealth apps because a single Download button can save a life and reshape health practices worldwide.








Dr Louise Corscadden acts as Conduct Science’s Director of Science and Development and Academic Technology Transfer. Her background is in genetics, microbiology, neuroscience, and climate chemistry.
