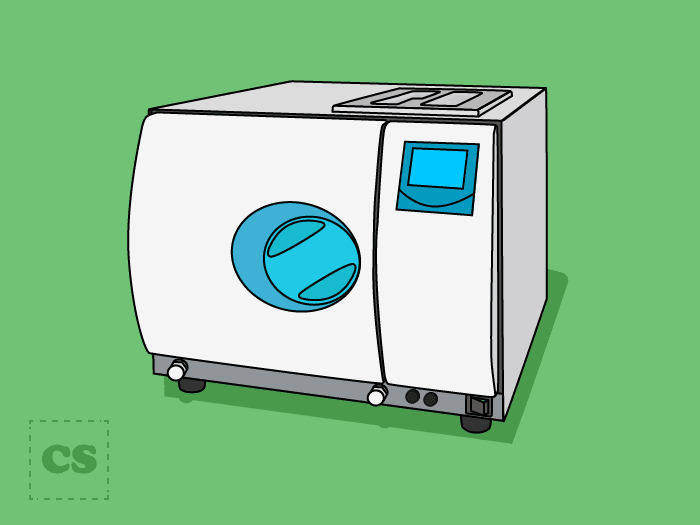
An autoclave sterilizes medical or laboratory equipment to kill viruses, bacteria, fungi, and spores. It is the most thorough kind of decontamination that employs saturated steam at a high temperature (typically 121°C) for 15-20 minutes for sterilization (Panta, Richardson, Shaw, Chambers, & Coope, 2019).
The steam must come into direct contact with the materials at the required temperature and pressure to be completely effective against microbes. This steam is highly pressurized, which allows its temperature to exceed 100°C, accounting for its efficiency. The amount of pressure and temperature the autoclave utilizes is inversely proportional to the time taken for sterilization. When the pressure is 108 kilopascals (kPa), the temperature of the steam is 121°C, and the time needed for sterilization is 20 minutes. On the other hand, at 206 kPa, the steam is 134°C, and it only takes 10 minutes for sterilization. (Dockery, 2012).
Charles Chamberland invented the autoclave in 1879. Researchers began to recognize the benefits of antiseptic surgery around the 1850s. Since then autoclaves have found usage in several fields such as research laboratories and animal labs.
The autoclave operates on the principle of moist heat sterilization, in which the material inside the chamber is sterilized by steam under high pressure.
The Autoclave is made to cater to sterilization requirements while being safe and fully automated.
All of the settings can be changed as per the laboratory’s needs.
Inadequate sterilization of medical and lab equipment increases the risk of infection from human to human and from the environment. Therefore, effective sterilization of lab and medical equipment is required.
Although autoclaves are typically used to decontaminate laboratory instruments and biological waste, they are also widely used for sterilizing animal feed, bedding, and enrichment items. Rodent meal is sterilized to prevent the entry of possibly harmful microbes that can cause diseases or latent infections, affecting physiological response. This method became popular as the requirement for specific pathogen-free animals grew.
Scientists have isolated gastrointestinal microorganisms from unsterilized, raw content rodent meals on some instances, notably Salmonella spp., E. coli, and Clostridium spp. Moreover, several recent reports involved the continuity of mouse parvovirus in mouse territories due to the use of an unsterilized diet. Organizations that autoclave their animal diets, on the other hand, should think about the temperatures required for feed sterilization as well as the kind of research in which these autoclaved diets are utilized (Kurtz et al., 2018).
Following are some of the precautions recommended while working with an autoclave:
Strengths:
The autoclave effectively sterilizes lab equipment using saturated steam. However, it also has a safety mechanism to avoid excessive pressure buildup. The water in the autoclave is brought to a lower temperature by the cooling system before being discharged to minimize damage to the facility’s sewerage system. Some autoclaves additionally have a suction mechanism to eliminate air before injecting steam. As materials containing water cannot be sterilized by dry heat sterilization, autoclaves are essential for ensuring their sterilization. Surgical tools, equipment, pharmaceutical instruments, microbial growth media, and other laboratory items are commonly sterilized using it. Solids and fluids can also be sterilized using this apparatus.
Limitations:
Although an autoclave is a trusted sterilizer, it may not be the best solution for every sterilization need. It cannot be used for heat-sensitive materials or sharp-edged instruments, especially high-grade carbon steel scissors and scalpel blade edges. Some things, such as fabric and linens, cannot be sterilized without being destroyed by the autoclave. High heat can cause some plasticware to melt, and sharp equipment can become dull. Furthermore, many compounds degrade during sterilization, and oily substances cannot be handled since they do not combine with water. Certain high-protein solutions, such as urea, vaccinations, and serums may need to be filtered without heat since they degrade in excessive heat.
An autoclave is an efficient and economical instrument used for sterilizing purposes in labs, healthcare, and dental settings. It works on the principle of steam sterilization. This high-pressurized steam is effective in killing microbes, including endospores. Although it is effective and recommended for many materials, it is not suitable for heat-sensitive, biological substances, plastic ware, and sharp objects.
Dockery, G. D. (2012). Chapter 7 – Aseptic techniques. In G. D. Dockery & M. E. Crawford (Eds.), Lower Extremity Soft Tissue & Cutaneous Plastic Surgery (Second Edition) (pp. 53-68). Oxford: W.B. Saunders.
Gillespie, E. H., & Gibbons, S. A. (1975). Autoclaves and their dangers and safety in laboratories. The Journal of hygiene, 75(3), 475-487. doi:10.1017/s0022172400024517
Kurtz, D. M., Glascoe, R., Caviness, G., Locklear, J., Whiteside, T., Ward, T., . . . Kissling, G. E. (2018). Acrylamide Production in Autoclaved Rodent Feed. Journal of the American Association for Laboratory Animal Science: JAALAS, 57(6), 703-711. doi:10.30802/AALAS-JAALAS-18-000011
Panta, G., Richardson, A. K., Shaw, I. C., Chambers, S., & Coope, P. A. (2019). Effectiveness of steam sterilization of reusable medical devices in primary and secondary care public hospitals in Nepal and factors associated with ineffective sterilization: A nation-wide cross-sectional study. PloS one, 14(11), e0225595-e0225595. doi:10.1371/journal.pone.0225595
Rutala, W. A., & Weber, D. J. (2015). Disinfection, Sterilization, and Control of Hospital Waste. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 3294-3309.e3294. doi:10.1016/B978-1-4557-4801-3.00301-5
What is Autoclaving? Retrieved from https://www.qorpak.com/pages/autoclaving