Definition: Bring your own device (BYOD) has become a leading approach in healthcare settings. BYOD is a term that refers to the implementation of patients’ own mobile devices in clinical trials and healthcare practice. Note that only in the US, 95% of people own a cell phone, while 75% own a computer. From smartphones to laptops, the BYOD movement embraces the latest innovations in mobiles solutions and technological services to engage participants and clinicians. With increased familiarity and reduced costs, BYOD can facilitate patient-doctor communication and interoperability.
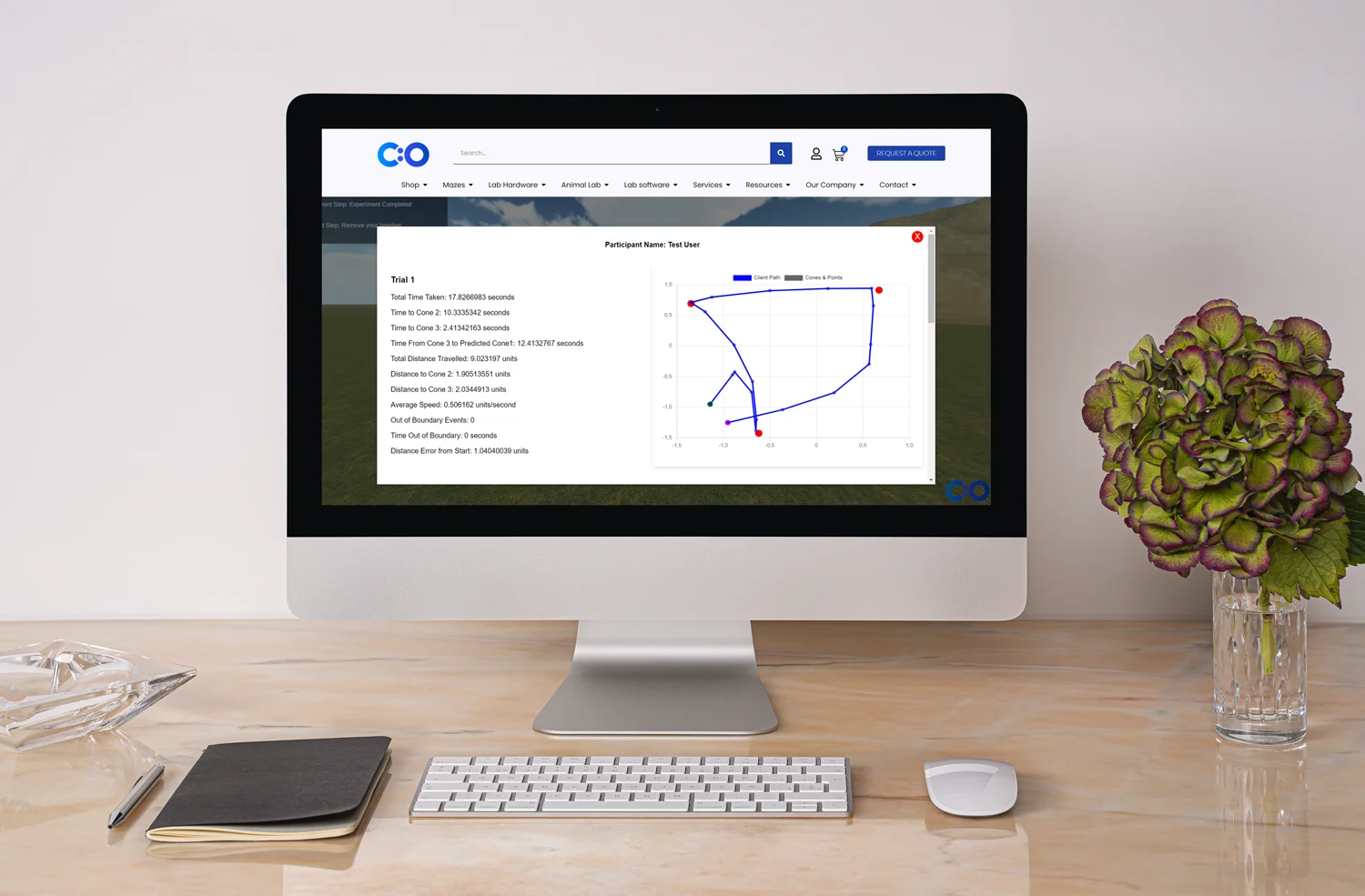
The transition from paper-based to electronic data: There’s no doubt that mobile technology facilitates doctor-patient communication, data collection, and statistical analysis. In fact, according to data, 80% of healthcare workers use tablets in practice, followed by smartphones (42%). With the inevitable transition from paper-based to electronic data, it’s no surprise that a vast majority of experts and sponsors turn to electronic clinical outcome assessments (eCOA) (“9 Key Factors to Evaluate When Considering BYOD”). Although provisioned devices (provided to the subjects) are still widely used to collect electronic data, the use of BYOD in healthcare research and practice is increasing in popularity.
History of BYOD and IT consumerization: Interestingly, BYOD in healthcare settings is not an isolated phenomenon. Since mobile technologies have become an integrated part of people’s lives, the consumerization of information technology (IT) is more than logical. We should mention that the term BYOD was introduced in 2004 when a voice over Internet Protocol (VoIP) service allowed businesses to use their own devices. In 2009, companies started allowing employees to bring and connect their own mobile devices to work. Two years later, BYOD became a leading term in marketing strategies, marking the new consumer enterprise. Note that BYOD can lead to an increase in productivity and a decrease in hardware costs. In addition, research shows that BYOD has numerous benefits across educational settings, as well as other industries.
Benefits of BYOD: BYOD is an effective approach in healthcare settings and clinical trials as it allows subjects to provide medical information via their own internet-enabled device. It’s not a secret that recruiting participants and collecting data are among the most challenging aspects of research. With numerous benefits, BYOD is preferred over traditional methods. For instance, users can either access an online platform or download a medical app. The BYOD approach has been implemented even in Phase II and Phase III clinical trials. Some of the major benefits include:
Challenges in the implementation of BYOD: Although BYOD is increasing in popularity, there are a few challenges researchers need to overcome in order to implement BYOD in clinical trials (Marshall, 2014). Researchers need to create a good study design, taking into account patient rapport, data accuracy, and technical aspects (e.g., screen size). Factors, such as lack of a mobile device, demographics, reimbursement, and IT use support, should also be considered. Note that one of the major concerns is data security and HIPAA regulations.
Risks associated with BYOD: Possible risks in clinical research are alarming. Data security and patient privacy are among the major concerns. Since medical data is sensitive, networks must be protected. Virtual sandboxes can be installed on a device to protect apps that deal with medical data. Thus, clinicians won’t breach HIPAA policies, support staff won’t access certain services, and patients will access a hospital’s patient portal only for relevant information.
BYOD in healthcare practice and aspects to consider: With its numerous benefits, BYOD is becoming one of the most effective approaches in research. When implementing BYOD in practice, clinicians and IT specialists should consider the following aspects in order to overcome challenges and possible risks (“9 Key Factors to Evaluate When Considering BYOD”):
BYOD checklist: Creating a good study design is one of the major factors for scientific success. Apart from the aspects described above, researchers should consider the following checklist (“9 Key Factors to Evaluate When Considering BYOD”):
Clinical trials with BYOD: Research proves that BYOD is an effective approach in practice, considering patient management, compliance, and satisfaction. Based on Google Analytics, the findings from the randomized trial described earlier revealed that the BYOD subgroup showed higher engagement with the intervention, more application sessions per day, and longer sessions. Interestingly, the BYOD subgroup showed a significant effect of engagement on drug compliance in the end-line period of the trial. In fact, interviews revealed that BYOD users found it easy to integrate the mobile application into their daily routines (Pugliese et al., 2016).
With the effects of IT consumerization in real life, there’s no doubt that technology facilitates industries. Mobile devices have become an integrated part of people’s lives and business strategies. In healthcare, in particular, BYOD can lead to an increase in productivity, engagement, compliance, high-quality data, real-life communication, and cost-effective research. By considering data type, BYOD-related training, demographics, and privacy risks, experts can manage the successful implementation of BYOD in clinical trials in accordance with safety and ethical regulations.
Most of all, BYOD can improve user experience and well-being. Patients can bring their own device, which eliminates the need for carrying an additional device or training. Real-life data, smooth doctor-patient communication, and online support can only improve patient outcomes and quality of life. In the end, patients are the core of research and digital health.
Bol, N. Helberger, N., & Weert, J. (2018). Differences in mobile health app use: A source of new digital inequalities? The Information Society: An International Society, 34 (3).
Pugliese, L., Woodriff, M., Crowley, O., Lam, V., Sohn, J., & Bradley, S. (2016). Feasibility of the “Bring Your Own Device” Model in Clinical Research: Results from a Randomized Controlled Pilot Study of a Mobile Patient Engagement Tool. Cureus, 8 (3).
Marshall, S. (2014). IT Consumerization: A Case Study of BYOD in a Healthcare Setting. Retrieved from https://timreview.ca/article/771
9 Key Factors to Evaluate When Considering BYOD. Retrieved from https://resources.crfhealth.com/ebooks/9-key-factors-to-evaluate-when-considering-byod





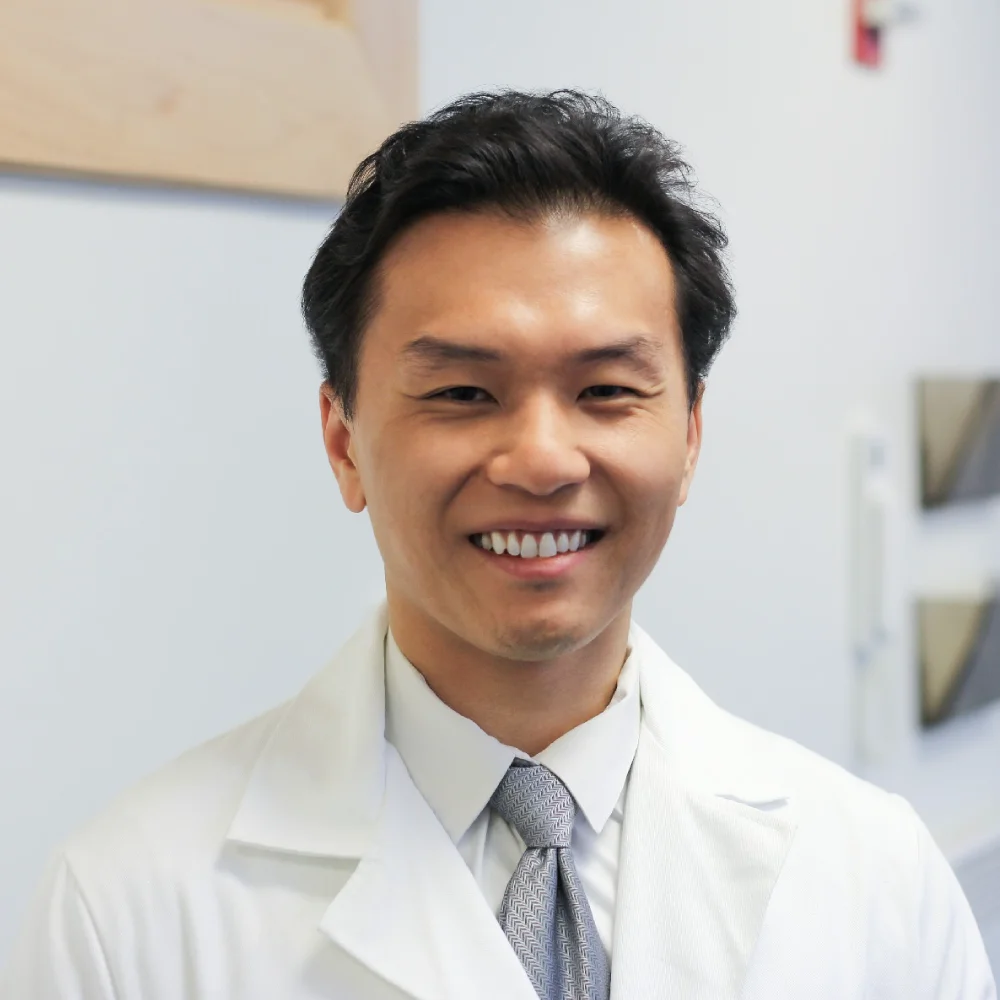
Shuhan He, MD is a dual-board certified physician with expertise in Emergency Medicine and Clinical Informatics. Dr. He works at the Laboratory of Computer Science, clinically in the Department of Emergency Medicine and Instructor of Medicine at Harvard Medical School. He serves as the Program Director of Healthcare Data Analytics at MGHIHP. Dr. He has interests at the intersection of acute care and computer science, utilizing algorithmic approaches to systems with a focus on large actionable data and Bayesian interpretation. Committed to making a positive impact in the field of healthcare through the use of cutting-edge technology and data analytics.