

Medical research revolves around challenging ideas, practical solutions, and optimistic results. However, even the most promising clinical trial can collapse if it faces poor management practices. Since medical research is a complicated and sensitive process, it requires expert management (Farrell et al., 2011). High standards can be achieved only via careful planning, good management, and regular collaboration between experts.
As a matter of fact, there are several aspects researchers need to consider prior to conducting a study to ensure good management practices and high standards (Peat, 2011):
Although medical teams play a leading role in research, monitoring committees are also needed to ensure good management practices. In fact, creating a hierarchy of committees, whose role will be decided before conducting the study, is one of the most effective practices (Peat, 2011). While internal committees include investigators and staff, external committees consist of peers and other experts. Independent experts are a must: they can help researchers decide on the number of interim analyses, and they can support integrity. Note that there must be a committee that should be responsible particularly for data analyses.
Regular closed meetings are crucial for good management, decision-making, and quality of data. Last but not the least, presentations and discussions (on both national and international levels) can facilitate the multi-centered approach which is needed in research (Farrell et al., 2010).
Medical research is a diverse field of work, but in the end, research teams are the most active participants in any clinical trial. In fact, managing research teams do not differ from managing business teams. Good teams consist of professionals with different expertise; therefore, diversity should be promoted to create a productive environment. To be more precise, each medical team includes numerous experts, such as a chief investigator, a trial manager, a data manager, administrative staff, statisticians, and programmers.
Training is also mandatory in various aspects, such as recruitment and data entry. On the other hand, all roles should be well-defined, and staff should be able to take responsibility for their actions. The most important aspect is to create an atmosphere marked by personal satisfaction and a friendly attitude.
The study coordinator motivates the staff and encourages research. The study coordinator should be familiar with all aspects of research and staff roles to promote high standards and integrity. From organizing paperwork by checking data entries to talking directly with participants – the study coordinator should be a knowledgeable person passionate about the project.
People who manage medical research must have excellent communication and organization skills and must express enthusiasm and innovative thinking. Managers must encourage professional development and personal satisfaction at the same time. They must create a level of trust and a balance between realistic priorities and interesting tasks. Most of all, good managers must celebrate research success.
Let’s not forget that clinical trials rely on data. Recruiting participants and collecting data is challenging, and so are data entry and analysis. Here are some basic principles and steps of managing medical information experts must consider:
After data collection, all results must be entered into a database. Creating a good database design is difficult, but it’s a process that can spare lots of effort and errors at the later stages of any analysis. When planning a design, the type and the size of the tested variables need to be considered prior to research.
Checking for errors is fundamental. Cross-checks can help experts spot values that are outside the utilized ranges and which consequently can’t be used in the analysis (Peat, 2011).
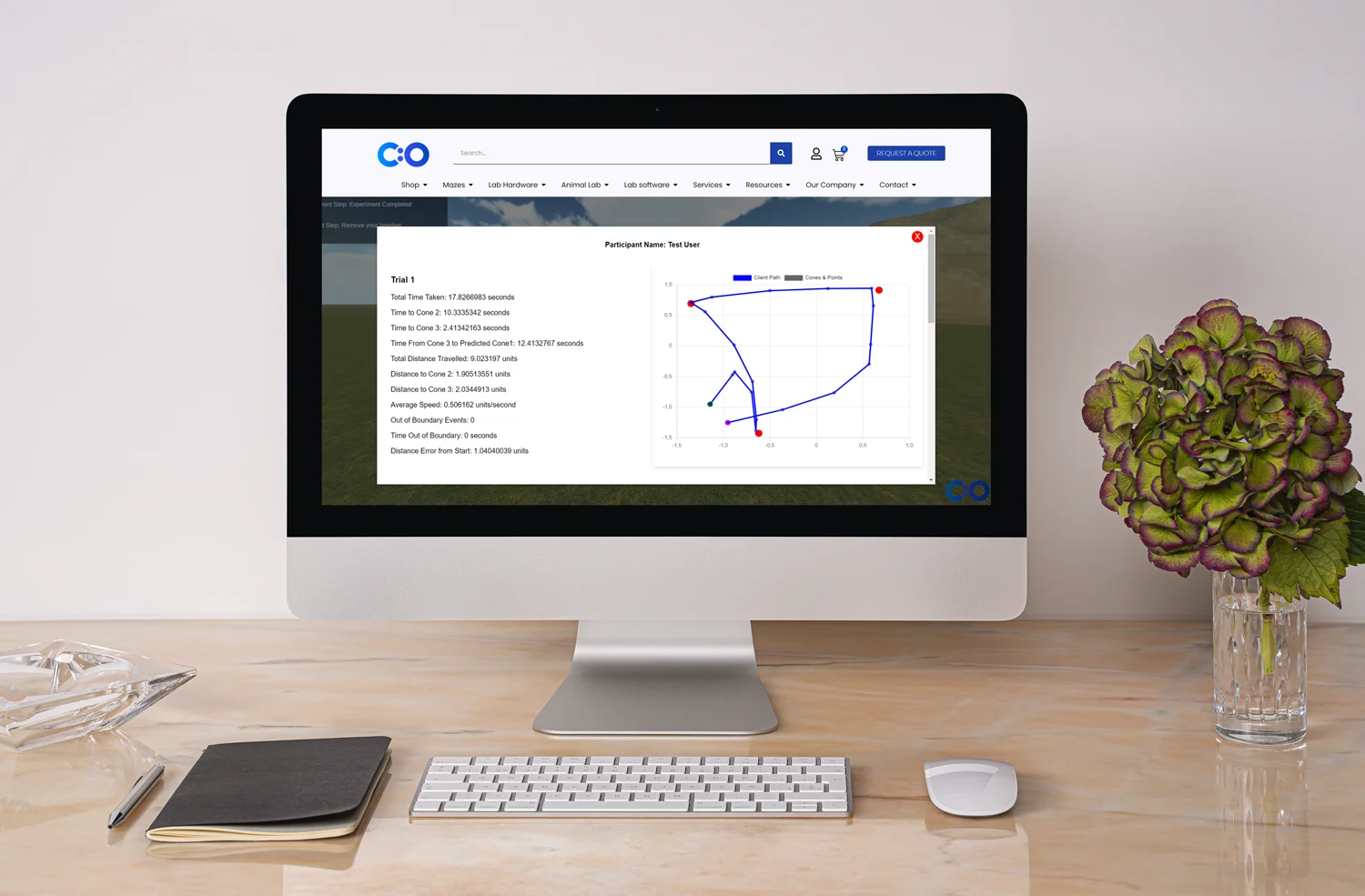
The actual process of data entry is also prone to errors. Self-coding questionnaires are easier to analyze. Nevertheless, any research team must agree on either alphabetic or numeric information prior to research. As explained above, range checks, visual checks, and cross-checks are a must. Also, good management should ensure that the entered data will be verified by another coordinator. Note that research staff should be blinded to the study results to avoid errors and bias. Once again, all errors should be documented in the data management manual of the study (Peat, 2011). If there are missing data, a beneficial approach is to contact subjects to clarify or expand on the missing information. When more than one instrument has been utilized, several records should be created. Note that these records should match on at least two indicators to ensure integrity and validity of data (e.g., name and number). Often commercial software can be utilized to support researchers in data analysis; such programs adopt a precise and complete approach to data management.
In today’s digital health era, connectivity software and relational databases can be highly beneficial, especially when compared to Excel or Word tables. Such programs allow statistical packages to analyze the collected data directly – without having data exported and then imported again. This guarantees transparency and precision. On top of that, a read-only mode can be implemented, which ensures the safety and integrity of data management.
However, some studies can’t access such facilities. When connectivity software or relational databases are not available, abbreviated files and spreadsheets can be created to export data and then analyze it (Peat, 2011). During this process, all changes must be monitored in the main file, so the master database will be able to reach high standards and integrity.
When we talk about data management, the safety of data should always be the main aim of the research. Technical issues, accidents, and theft happen, so backup files are also needed. It’s a good idea to archive files. Note that often computer departments deal with security and technical issues.
Medical information should support interoperability and collaboration, but safety is vital. Thus, rights can be restricted and read-only modes created. Confidentiality should also be considered, especially when it comes to pediatric populations and rare diseases. In fact, in some working files, all information about the subjects may be excluded to prevent administrative clerks from having access to people’s data (Peat, 2011).
Management practices in medical research are paramount. Experts need guidance because clinical trials are complex, expensive, and time-consuming studies. Researchers should never rush or force participants. Quite the opposite: researchers should plan the study carefully and create a good working environment.
Good management practices imply that tasks and goals are clear way before the actual execution and analysis. All aspects of research must be planned in advance. Good planning means minimal work for participants and investigators. Technology is also fundamental: for instance, digital recruiting methods and online data forms can facilitate research. Note that when it comes to digital solutions, good managers should provide training to staff.
Most of all, good management practices must ensure that staff feels appreciated, driven, and motivated. Not surprisingly, communication and collaboration are paramount. In the end, medical findings should not be restricted to a single organization – but to patients all over the world.
To sum up, despite the field of work – from clinical trials to business conglomerates – good management practices are vital to help teams succeed.
Farrell, B., Kenyon, S., Shakur, H. (2010). Managing clinical trials. BioMed Central.
Peat, J. (2011). Conducting the Study. Health Science Research, SAGE Publications, Ltd.









Shuhan He, MD is a dual-board certified physician with expertise in Emergency Medicine and Clinical Informatics. Dr. He works at the Laboratory of Computer Science, clinically in the Department of Emergency Medicine and Instructor of Medicine at Harvard Medical School. He serves as the Program Director of Healthcare Data Analytics at MGHIHP. Dr. He has interests at the intersection of acute care and computer science, utilizing algorithmic approaches to systems with a focus on large actionable data and Bayesian interpretation. Committed to making a positive impact in the field of healthcare through the use of cutting-edge technology and data analytics.
